Vitrectomy in PDR
Improved techniques and equipment are driving earlier vitrectomy in proliferative diabetic retinopathy

Dermot McGrath
Published: Friday, February 1, 2019
[caption id="attachment_14112" align="alignleft" width="623"]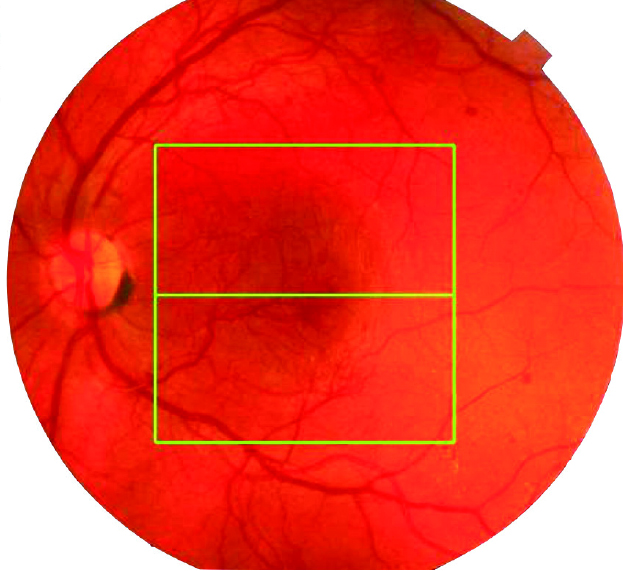 Florid proliferative diabetic retinopathy: such cases may be better with a vitrectomy before they develop either traction or a vitreous haemorrhage[/caption]
Improved techniques, along with major advances in minimally invasive vitreoretinal surgery and the use of intravitreal bevacizumab, are all driving a trend towards earlier vitrectomy in proliferative diabetic retinopathy, according to Alistair Laidlaw MD FRCS FRCOphth.
“About 20% of diabetics will benefit from a vitrectomy at some point for non-clearing vitreous haemorrhage or tractional retinal detachment. It is much safer than it was before and it is getting better still. The use of anti-VEGF injections has been a game-changer in that respect, but pre-existing macular damage still limits the visual outcome,” Dr Laidlaw told delegates attending the 8th EURETINA Winter Meeting in Budapest.
Dr Laidlaw added that there may also be a case for pre-emptive vitrectomy in selected florid high-risk PDR cases in order to prevent the angio-fibrotic switch and subsequent traction, and thereby improve visual outcomes.
In a broad overview of the evolution of pars plana vitrectomy (PPV) in PDR over the past 30 years, Dr Laidlaw, Consultant Ophthalmic Surgeon at St Thomas’ Hospital London, United Kingdom, explained that the classic role of surgery for diabetic retinopathy was defined in 1985 by the Diabetic Retinopathy Vitrectomy Study (DRVS).
That study randomised 616 eyes with recent vitreous haemorrhage and visual acuity of 5/200 or less for at least one month, to undergo early vitrectomy within six months versus observation. The greatest benefit from surgery was found in type 1 diabetics, who tended to be younger and had more severe disease, whereas no such advantage was found in the type 2 diabetes group.
While the DRVS study showed the benefits of early PPV in vitreous haemorrhage, with greater probability of visual acuity improvement or stabilisation, a disturbingly large proportion of patients ended up with no light perception, said Dr Laidlaw.
“The study did show that you were a bit better off having a vitrectomy at one and two years, but with 20% rates of no perception of light. This means that you were as likely to go completely blind as you were to get back 6/12, so it was not a particularly good advert for vitrectomy in diabetic patients,” he said.
With improved surgical techniques and instrumentation, the results of Diabetic PPV have considerably improved compared to the DRVS era, noted Dr Laidlaw.
“It is completely different now. We now have routine endolaser, and we are in the era of small-gauge vitreoretinal surgery, with improved fluidics and high-performance vitreous cutters. We can stain the retina for better visibility, and we have chandelier lighting and wide-angle viewing systems. We also have bimanual surgery and anti-VEGF augmentation to enhance surgery. We also have a certain corporate experience now with so many surgeons who have performed vitrectomies that it has inevitably got better,” he said.
The enhanced surgical environment is reflected in more recent results for PPV in diabetic patients, said Dr Laidlaw.
Data from the UK’s National Ophthalmology Database report on diabetic vitrectomy, which looked at 939 eyes of 834 patients who underwent primary vitrectomy for PDR between 2001 and 2010, showed that of 420 eyes that underwent vitrectomy without delamination the intraoperative complication rate was 13.1%, with 30% of eyes requiring an intravitreal tamponade and 11.7% undergoing further vitrectomy. Almost 18% of 127 phakic eyes developed cataracts within a year, with 63.6% achieving visual success and 8.2% visual loss.
Of the 519 eyes that underwent vitrectomy with delamination, the intraoperative complication rate was 30.4%, with 57.6% requiring an intravitreal tamponade and 15.0% undergoing further vitrectomy. Just over 21% of 126 phakic eyes developed cataracts within a year, with 62.8% achieving visual success and 14.9% visual loss.
“This study showed the results are pretty good – there were not more patients without light perception at the end of the study compared to before the study, and the visual acuity got a lot better for the majority of patients. One of the key messages to emerge from this is that you don’t get the vision back if the retina is already crunched up, so there may be a case for earlier intervention,” he said.
[caption id="attachment_14113" align="alignleft" width="994"]
Florid proliferative diabetic retinopathy: such cases may be better with a vitrectomy before they develop either traction or a vitreous haemorrhage[/caption]
Improved techniques, along with major advances in minimally invasive vitreoretinal surgery and the use of intravitreal bevacizumab, are all driving a trend towards earlier vitrectomy in proliferative diabetic retinopathy, according to Alistair Laidlaw MD FRCS FRCOphth.
“About 20% of diabetics will benefit from a vitrectomy at some point for non-clearing vitreous haemorrhage or tractional retinal detachment. It is much safer than it was before and it is getting better still. The use of anti-VEGF injections has been a game-changer in that respect, but pre-existing macular damage still limits the visual outcome,” Dr Laidlaw told delegates attending the 8th EURETINA Winter Meeting in Budapest.
Dr Laidlaw added that there may also be a case for pre-emptive vitrectomy in selected florid high-risk PDR cases in order to prevent the angio-fibrotic switch and subsequent traction, and thereby improve visual outcomes.
In a broad overview of the evolution of pars plana vitrectomy (PPV) in PDR over the past 30 years, Dr Laidlaw, Consultant Ophthalmic Surgeon at St Thomas’ Hospital London, United Kingdom, explained that the classic role of surgery for diabetic retinopathy was defined in 1985 by the Diabetic Retinopathy Vitrectomy Study (DRVS).
That study randomised 616 eyes with recent vitreous haemorrhage and visual acuity of 5/200 or less for at least one month, to undergo early vitrectomy within six months versus observation. The greatest benefit from surgery was found in type 1 diabetics, who tended to be younger and had more severe disease, whereas no such advantage was found in the type 2 diabetes group.
While the DRVS study showed the benefits of early PPV in vitreous haemorrhage, with greater probability of visual acuity improvement or stabilisation, a disturbingly large proportion of patients ended up with no light perception, said Dr Laidlaw.
“The study did show that you were a bit better off having a vitrectomy at one and two years, but with 20% rates of no perception of light. This means that you were as likely to go completely blind as you were to get back 6/12, so it was not a particularly good advert for vitrectomy in diabetic patients,” he said.
With improved surgical techniques and instrumentation, the results of Diabetic PPV have considerably improved compared to the DRVS era, noted Dr Laidlaw.
“It is completely different now. We now have routine endolaser, and we are in the era of small-gauge vitreoretinal surgery, with improved fluidics and high-performance vitreous cutters. We can stain the retina for better visibility, and we have chandelier lighting and wide-angle viewing systems. We also have bimanual surgery and anti-VEGF augmentation to enhance surgery. We also have a certain corporate experience now with so many surgeons who have performed vitrectomies that it has inevitably got better,” he said.
The enhanced surgical environment is reflected in more recent results for PPV in diabetic patients, said Dr Laidlaw.
Data from the UK’s National Ophthalmology Database report on diabetic vitrectomy, which looked at 939 eyes of 834 patients who underwent primary vitrectomy for PDR between 2001 and 2010, showed that of 420 eyes that underwent vitrectomy without delamination the intraoperative complication rate was 13.1%, with 30% of eyes requiring an intravitreal tamponade and 11.7% undergoing further vitrectomy. Almost 18% of 127 phakic eyes developed cataracts within a year, with 63.6% achieving visual success and 8.2% visual loss.
Of the 519 eyes that underwent vitrectomy with delamination, the intraoperative complication rate was 30.4%, with 57.6% requiring an intravitreal tamponade and 15.0% undergoing further vitrectomy. Just over 21% of 126 phakic eyes developed cataracts within a year, with 62.8% achieving visual success and 14.9% visual loss.
“This study showed the results are pretty good – there were not more patients without light perception at the end of the study compared to before the study, and the visual acuity got a lot better for the majority of patients. One of the key messages to emerge from this is that you don’t get the vision back if the retina is already crunched up, so there may be a case for earlier intervention,” he said.
[caption id="attachment_14113" align="alignleft" width="994"]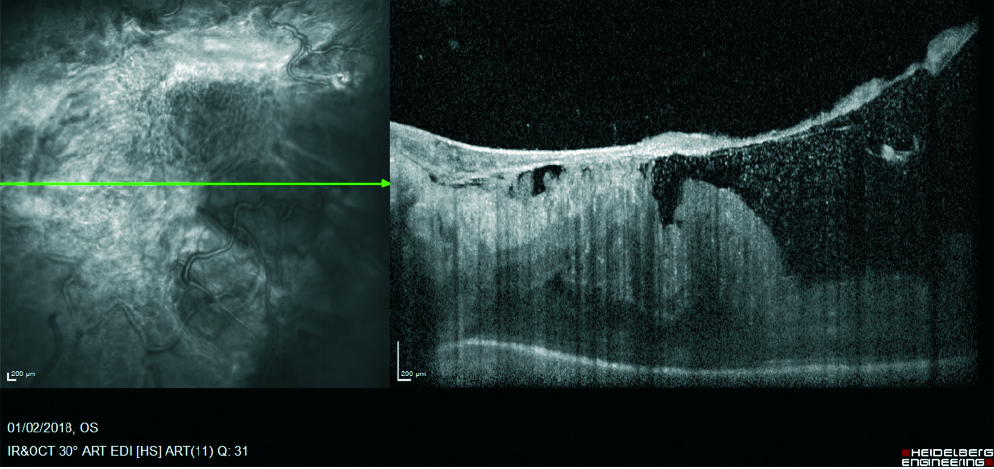 OCT showing severe tractional complications of proliferative diabetic retinopathy: ideally we would prevent such complications occurring[/caption]
In the DRIVE UK study, which identified 185 eyes of 158 patients who underwent vitrectomy from January 2007 to December 2009 due to diabetes-related complications, 50% of the eyes with tractional retinal detachment and non-clearing vitreous haemorrhage, and 87% of the eyes with non-clearing vitreous haemorrhage, improved by at least three ETDRS lines at 12 months, said Dr Laidlaw.
Recent studies have shown that pre-treatment of anti-VEGF agents before vitrectomy for complicated PDR facilitates surgery, with less early recurrent vitreous haemorrhage and quicker absorption of recurrent vitreous haemorrhage.
“This really has been a game-changer if you are going to have to manipulate the retinal surface. With anti-VEGF in the eye prior to surgery, the difference is like removing sticky tape off a table top compared to taking chewing gum off wet newspaper. It makes the surgery so much easier, with less bleeding and easier fibrovascular membrane dissection,” he concluded.
Alistair Laidlaw: alistair.laidlaw@gstt.nhs.uk
OCT showing severe tractional complications of proliferative diabetic retinopathy: ideally we would prevent such complications occurring[/caption]
In the DRIVE UK study, which identified 185 eyes of 158 patients who underwent vitrectomy from January 2007 to December 2009 due to diabetes-related complications, 50% of the eyes with tractional retinal detachment and non-clearing vitreous haemorrhage, and 87% of the eyes with non-clearing vitreous haemorrhage, improved by at least three ETDRS lines at 12 months, said Dr Laidlaw.
Recent studies have shown that pre-treatment of anti-VEGF agents before vitrectomy for complicated PDR facilitates surgery, with less early recurrent vitreous haemorrhage and quicker absorption of recurrent vitreous haemorrhage.
“This really has been a game-changer if you are going to have to manipulate the retinal surface. With anti-VEGF in the eye prior to surgery, the difference is like removing sticky tape off a table top compared to taking chewing gum off wet newspaper. It makes the surgery so much easier, with less bleeding and easier fibrovascular membrane dissection,” he concluded.
Alistair Laidlaw: alistair.laidlaw@gstt.nhs.uk
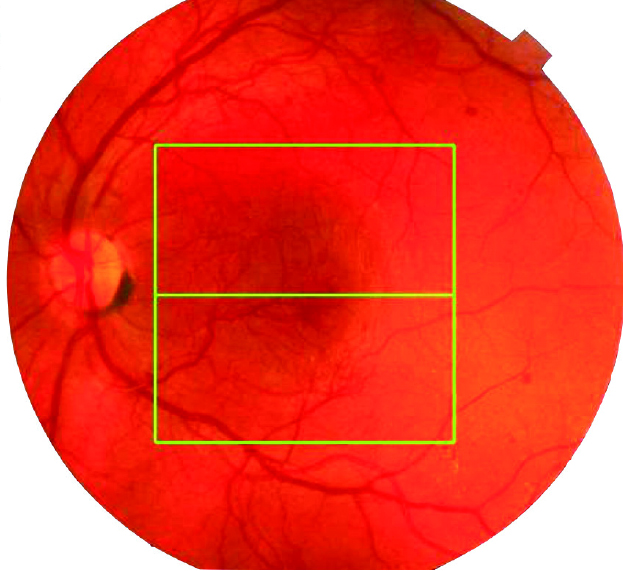 Florid proliferative diabetic retinopathy: such cases may be better with a vitrectomy before they develop either traction or a vitreous haemorrhage[/caption]
Improved techniques, along with major advances in minimally invasive vitreoretinal surgery and the use of intravitreal bevacizumab, are all driving a trend towards earlier vitrectomy in proliferative diabetic retinopathy, according to Alistair Laidlaw MD FRCS FRCOphth.
“About 20% of diabetics will benefit from a vitrectomy at some point for non-clearing vitreous haemorrhage or tractional retinal detachment. It is much safer than it was before and it is getting better still. The use of anti-VEGF injections has been a game-changer in that respect, but pre-existing macular damage still limits the visual outcome,” Dr Laidlaw told delegates attending the 8th EURETINA Winter Meeting in Budapest.
Dr Laidlaw added that there may also be a case for pre-emptive vitrectomy in selected florid high-risk PDR cases in order to prevent the angio-fibrotic switch and subsequent traction, and thereby improve visual outcomes.
In a broad overview of the evolution of pars plana vitrectomy (PPV) in PDR over the past 30 years, Dr Laidlaw, Consultant Ophthalmic Surgeon at St Thomas’ Hospital London, United Kingdom, explained that the classic role of surgery for diabetic retinopathy was defined in 1985 by the Diabetic Retinopathy Vitrectomy Study (DRVS).
That study randomised 616 eyes with recent vitreous haemorrhage and visual acuity of 5/200 or less for at least one month, to undergo early vitrectomy within six months versus observation. The greatest benefit from surgery was found in type 1 diabetics, who tended to be younger and had more severe disease, whereas no such advantage was found in the type 2 diabetes group.
While the DRVS study showed the benefits of early PPV in vitreous haemorrhage, with greater probability of visual acuity improvement or stabilisation, a disturbingly large proportion of patients ended up with no light perception, said Dr Laidlaw.
“The study did show that you were a bit better off having a vitrectomy at one and two years, but with 20% rates of no perception of light. This means that you were as likely to go completely blind as you were to get back 6/12, so it was not a particularly good advert for vitrectomy in diabetic patients,” he said.
With improved surgical techniques and instrumentation, the results of Diabetic PPV have considerably improved compared to the DRVS era, noted Dr Laidlaw.
“It is completely different now. We now have routine endolaser, and we are in the era of small-gauge vitreoretinal surgery, with improved fluidics and high-performance vitreous cutters. We can stain the retina for better visibility, and we have chandelier lighting and wide-angle viewing systems. We also have bimanual surgery and anti-VEGF augmentation to enhance surgery. We also have a certain corporate experience now with so many surgeons who have performed vitrectomies that it has inevitably got better,” he said.
The enhanced surgical environment is reflected in more recent results for PPV in diabetic patients, said Dr Laidlaw.
Data from the UK’s National Ophthalmology Database report on diabetic vitrectomy, which looked at 939 eyes of 834 patients who underwent primary vitrectomy for PDR between 2001 and 2010, showed that of 420 eyes that underwent vitrectomy without delamination the intraoperative complication rate was 13.1%, with 30% of eyes requiring an intravitreal tamponade and 11.7% undergoing further vitrectomy. Almost 18% of 127 phakic eyes developed cataracts within a year, with 63.6% achieving visual success and 8.2% visual loss.
Of the 519 eyes that underwent vitrectomy with delamination, the intraoperative complication rate was 30.4%, with 57.6% requiring an intravitreal tamponade and 15.0% undergoing further vitrectomy. Just over 21% of 126 phakic eyes developed cataracts within a year, with 62.8% achieving visual success and 14.9% visual loss.
“This study showed the results are pretty good – there were not more patients without light perception at the end of the study compared to before the study, and the visual acuity got a lot better for the majority of patients. One of the key messages to emerge from this is that you don’t get the vision back if the retina is already crunched up, so there may be a case for earlier intervention,” he said.
[caption id="attachment_14113" align="alignleft" width="994"]
Florid proliferative diabetic retinopathy: such cases may be better with a vitrectomy before they develop either traction or a vitreous haemorrhage[/caption]
Improved techniques, along with major advances in minimally invasive vitreoretinal surgery and the use of intravitreal bevacizumab, are all driving a trend towards earlier vitrectomy in proliferative diabetic retinopathy, according to Alistair Laidlaw MD FRCS FRCOphth.
“About 20% of diabetics will benefit from a vitrectomy at some point for non-clearing vitreous haemorrhage or tractional retinal detachment. It is much safer than it was before and it is getting better still. The use of anti-VEGF injections has been a game-changer in that respect, but pre-existing macular damage still limits the visual outcome,” Dr Laidlaw told delegates attending the 8th EURETINA Winter Meeting in Budapest.
Dr Laidlaw added that there may also be a case for pre-emptive vitrectomy in selected florid high-risk PDR cases in order to prevent the angio-fibrotic switch and subsequent traction, and thereby improve visual outcomes.
In a broad overview of the evolution of pars plana vitrectomy (PPV) in PDR over the past 30 years, Dr Laidlaw, Consultant Ophthalmic Surgeon at St Thomas’ Hospital London, United Kingdom, explained that the classic role of surgery for diabetic retinopathy was defined in 1985 by the Diabetic Retinopathy Vitrectomy Study (DRVS).
That study randomised 616 eyes with recent vitreous haemorrhage and visual acuity of 5/200 or less for at least one month, to undergo early vitrectomy within six months versus observation. The greatest benefit from surgery was found in type 1 diabetics, who tended to be younger and had more severe disease, whereas no such advantage was found in the type 2 diabetes group.
While the DRVS study showed the benefits of early PPV in vitreous haemorrhage, with greater probability of visual acuity improvement or stabilisation, a disturbingly large proportion of patients ended up with no light perception, said Dr Laidlaw.
“The study did show that you were a bit better off having a vitrectomy at one and two years, but with 20% rates of no perception of light. This means that you were as likely to go completely blind as you were to get back 6/12, so it was not a particularly good advert for vitrectomy in diabetic patients,” he said.
With improved surgical techniques and instrumentation, the results of Diabetic PPV have considerably improved compared to the DRVS era, noted Dr Laidlaw.
“It is completely different now. We now have routine endolaser, and we are in the era of small-gauge vitreoretinal surgery, with improved fluidics and high-performance vitreous cutters. We can stain the retina for better visibility, and we have chandelier lighting and wide-angle viewing systems. We also have bimanual surgery and anti-VEGF augmentation to enhance surgery. We also have a certain corporate experience now with so many surgeons who have performed vitrectomies that it has inevitably got better,” he said.
The enhanced surgical environment is reflected in more recent results for PPV in diabetic patients, said Dr Laidlaw.
Data from the UK’s National Ophthalmology Database report on diabetic vitrectomy, which looked at 939 eyes of 834 patients who underwent primary vitrectomy for PDR between 2001 and 2010, showed that of 420 eyes that underwent vitrectomy without delamination the intraoperative complication rate was 13.1%, with 30% of eyes requiring an intravitreal tamponade and 11.7% undergoing further vitrectomy. Almost 18% of 127 phakic eyes developed cataracts within a year, with 63.6% achieving visual success and 8.2% visual loss.
Of the 519 eyes that underwent vitrectomy with delamination, the intraoperative complication rate was 30.4%, with 57.6% requiring an intravitreal tamponade and 15.0% undergoing further vitrectomy. Just over 21% of 126 phakic eyes developed cataracts within a year, with 62.8% achieving visual success and 14.9% visual loss.
“This study showed the results are pretty good – there were not more patients without light perception at the end of the study compared to before the study, and the visual acuity got a lot better for the majority of patients. One of the key messages to emerge from this is that you don’t get the vision back if the retina is already crunched up, so there may be a case for earlier intervention,” he said.
[caption id="attachment_14113" align="alignleft" width="994"]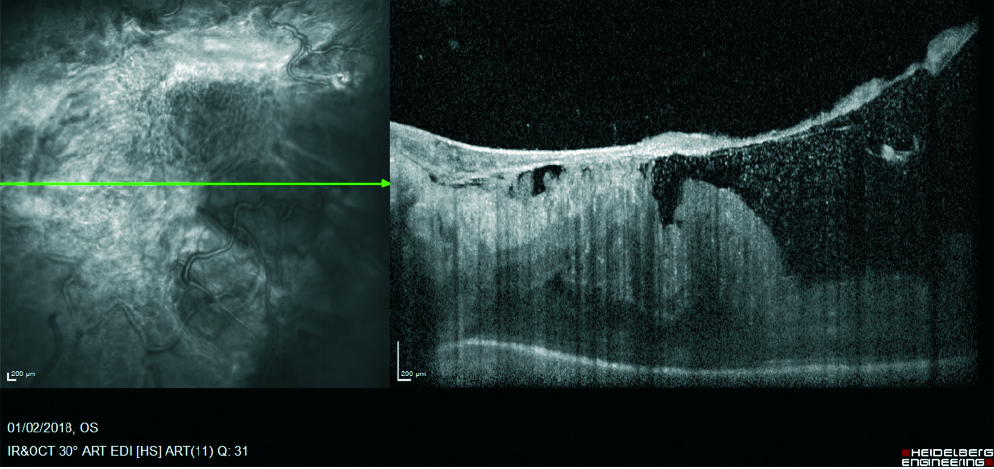 OCT showing severe tractional complications of proliferative diabetic retinopathy: ideally we would prevent such complications occurring[/caption]
In the DRIVE UK study, which identified 185 eyes of 158 patients who underwent vitrectomy from January 2007 to December 2009 due to diabetes-related complications, 50% of the eyes with tractional retinal detachment and non-clearing vitreous haemorrhage, and 87% of the eyes with non-clearing vitreous haemorrhage, improved by at least three ETDRS lines at 12 months, said Dr Laidlaw.
Recent studies have shown that pre-treatment of anti-VEGF agents before vitrectomy for complicated PDR facilitates surgery, with less early recurrent vitreous haemorrhage and quicker absorption of recurrent vitreous haemorrhage.
“This really has been a game-changer if you are going to have to manipulate the retinal surface. With anti-VEGF in the eye prior to surgery, the difference is like removing sticky tape off a table top compared to taking chewing gum off wet newspaper. It makes the surgery so much easier, with less bleeding and easier fibrovascular membrane dissection,” he concluded.
Alistair Laidlaw: alistair.laidlaw@gstt.nhs.uk
OCT showing severe tractional complications of proliferative diabetic retinopathy: ideally we would prevent such complications occurring[/caption]
In the DRIVE UK study, which identified 185 eyes of 158 patients who underwent vitrectomy from January 2007 to December 2009 due to diabetes-related complications, 50% of the eyes with tractional retinal detachment and non-clearing vitreous haemorrhage, and 87% of the eyes with non-clearing vitreous haemorrhage, improved by at least three ETDRS lines at 12 months, said Dr Laidlaw.
Recent studies have shown that pre-treatment of anti-VEGF agents before vitrectomy for complicated PDR facilitates surgery, with less early recurrent vitreous haemorrhage and quicker absorption of recurrent vitreous haemorrhage.
“This really has been a game-changer if you are going to have to manipulate the retinal surface. With anti-VEGF in the eye prior to surgery, the difference is like removing sticky tape off a table top compared to taking chewing gum off wet newspaper. It makes the surgery so much easier, with less bleeding and easier fibrovascular membrane dissection,” he concluded.
Alistair Laidlaw: alistair.laidlaw@gstt.nhs.uk
Tags: proliferative diabetic retinopathy
Latest Articles
A New High for Hyperopia
Hyperopia patients can expect a rise in the array of treatments.
Research Committee is Engine Driving the Future of ESCRS
Commitment to evidence-based medicine anchors studies and other projects.
ESCRS EPICAT Study Updates
Early results suggest subconjunctival 10 mg triamcinolone an effective strategy for dropless cataract surgery.
Second Global Consensus on Keratoconus
Forthcoming position paper to provide an updated and expanded view on evaluation and management.
Automating Cataract Surgery Assessment
AI system measures eye stability and centration in procedures.
Post-LASIK Tonometer Takes ESCRS Innovators Den Prize
Good ideas lead to solutions to unmet needs.
ESCRS forms Functional Vision Working Group
Expanding the Limits of KLEx
Hyperopia treatment receives CE approval; mixed astigmatism may follow.