Toric IOL implantation
In the first of two articles, Dr Soosan Jacob MS, FRCS, DNB highlights the relevance of posterior corneal astigmatism

Soosan Jacob
Published: Friday, July 31, 2020
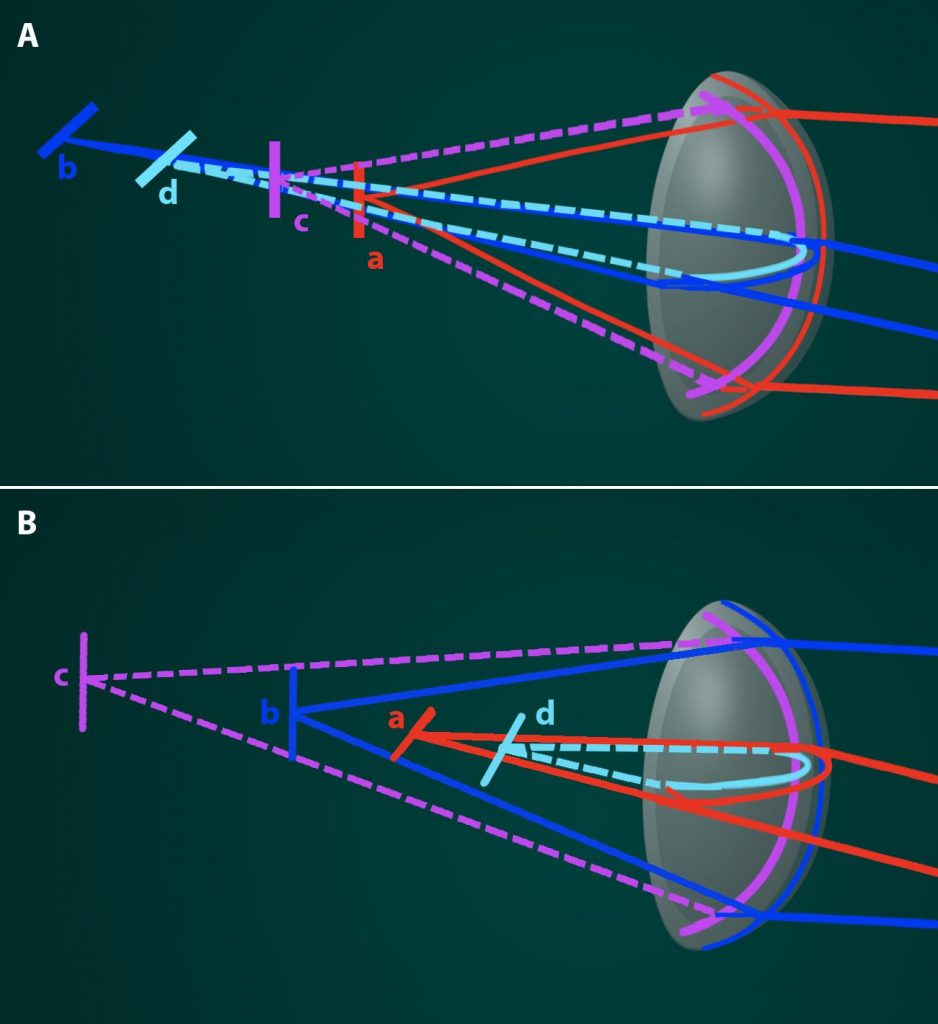 Refraction of incoming rays at the steep (red) and flat (blue) meridia on the anterior surface of an astigmatic cornea is shown. Irrespective of anterior corneal astigmatism, the posterior cornea generally has steep (pink) axis in the vertical meridian causing an against-the-rule astigmatism. The red and blue bold lines and the image lines “a” and “b” show refraction as would be presumed to occur without considering the effect of posterior corneal astigmatism (PCA). The light blue and pink dashed lines and image lines “c” and “d” show the actual refraction occurring at the posterior corneal surface. A Shows overestimation of WTR astigmatism that occurs if PCA is not taken into account. B Shows underestimation of ATR astigmatism that occurs if PCA is not taken into account.
Maximum refractive power of the eye is at the front surface of the cornea because of the significant difference in refractive indices between air and cornea. Keratometers and topographers give measurements of anterior corneal surface and thereby of anterior corneal astigmatism (ACA). However, we know now that despite the low difference in refractive indices of aqueous and stroma, posterior corneal astigmatism (PCA) does affect total corneal astigmatism (TCA), contributing an average of about 0.50 Dioptres (D) of against-therule (ATR) change.
TCA may be roughly calculated from ACA by using simplified Javal’s rule: “TCA=ATR_ACA@180o+ (+0.50@180o)” or “TCA=WTR_ACA@90o+ (-0.50@90o).”
This implies that TCA is generally less in case of with-the-rule (WTR) ACA and therefore using keratometric values alone can result in overestimation of the astigmatism by 0.5-to-0.6D and thereby an overcorrection.
Similarly, TCA is generally more in case of ATR ACA resulting in underestimation by 0.2-to-0.3D and under-correction of astigmatism if treatment is based on ACA alone. According to a 2009 study by Ho et al, PCA on an average caused reduction of TCA by 13.4% and in approximately 30% of eyes, PCA caused a change in TCA by >0.5D or by >10o in meridian from ACA.
For a long time, the reason for suboptimal results after toric IOL implantation was unclear and was attributed to lenticular astigmatism and even to the retina. However, recently, the posterior cornea has been studied in much greater detail. Koch et al’s paper from 2012 that analysed 715 corneas of 435 consecutive patients found that the steep corneal meridian was aligned vertically, between 60 and 120o in 51.9% of eyes for anterior surface and 86.6% of eyes for posterior surface. Since the posterior cornea is a negative lens, however, the vertically steep posterior curvature results in a net positive power in the horizontal direction or an ATR astigmatism.
They also found that with increasing WTR ACA, the PCA can also increase, even up to 1D. However, this is not the case with increasing ATR ACA, where mean PCA remains relatively same. In addition, with increasing age, the anterior cornea tended to change from WTR to ATR, yet this drift was not seen in the posterior cornea. A 2015 study by Hiyashi et al also showed an ATR drift of 0.2-to-0.4D in all age groups, during a 10-year follow-up in both post-cataract surgery as well as no surgery groups, with the drift further continuing over 20 years, as shown in their 2017 follow-up study.
Another interesting study was by Ueno et al, using swept-source OCT, which showed that the cornea is thicker along the vertical than the horizontal meridian, and this could contribute to ATR astigmatism by creating a steeper vertical cornea posteriorly. This difference was found to increase with age, which could partially account for the ATR drift in old age. Another finding was that the superior cornea was thicker than the inferior cornea and could possibly contribute to some higher-order aberrations.
MEASUREMENT OF POSTERIOR CORNEAL ASTIGMATISM
This may be done by newer and better tomographers, such as Scheimpflug imaging, slit scanning, OCT and reflective LED imaging, that allow measurement of the posterior cornea. However, accurate measurement of the posterior corneal curvature is still not possible and this led to the development and popularity of the Baylor nomogram. Another popular option is to use a theoretical approach such as used in the Barrett toric IOL calculator (www.ascrs.org).
BAYLOR NOMOGRAM
This regression approach based on population averages was proposed by Koch et al in their 2013 study to correct overestimation of WTR and underestimation of ATR. The surgically induced astigmatism (SIA- usually between 0.2 and 0.3D for most surgeons) is first factored in, followed by IOL’s spherical power and its position in the eye as these can affect the toricity at corneal plane. The nomogram then corrects for PCA by increasing or decreasing from that IOL power. It also factors in an additional adjustment to leave patients with slight WTR astigmatism to counter the ATR drift that occurs with ageing. These adjustments lead to a change in threshold for implanting toric IOLs to about 1.7D of WTR and 0.8D of ATR ACA after factoring in of SIA.
Many patients with oblique astigmatism may be considered to be midway in the age-related drift from WTR to ATR and these patients should be targeted on or only slightly below measured astigmatism. The toric IOL should therefore be aligned on axis or towards ATR axis and not towards the WTR axis in order to hold good for a longer time during the ATR drift.
BARRETT TORIC CALCULATOR
This incorporates the patient’s PCA and effective lens position (ELP) values rather than using population averages. However, it is based on a theoretical eye and PCA and ELP are predicted rather than measured though recent updates allow input of measured values as well. It uses anterior chamber depth (ACD), axial length, toricity ratio and SIA centroid for its calculations. For calculation of spherical equivalent IOL power, it bases itself on Barrett Universal II formula, where ACD is related to axial length and keratometry and principal plane of refraction of IOL is a variable. The Barrett True K Toric calculator is used in post-refractive surgery eyes.
Other formulae in use for toric IOL calculation include ASSORT calculator, Savini calculator, Holladay IOL consultant software etc.
To conclude, PCA is important for estimating power of the toric IOL to be implanted. IOL with less toricity needs to be chosen when correcting WTR astigmatism and conversely, more toricity when correcting ATR astigmatism.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India and can be reached at dr_soosanj@hotmail.com
Refraction of incoming rays at the steep (red) and flat (blue) meridia on the anterior surface of an astigmatic cornea is shown. Irrespective of anterior corneal astigmatism, the posterior cornea generally has steep (pink) axis in the vertical meridian causing an against-the-rule astigmatism. The red and blue bold lines and the image lines “a” and “b” show refraction as would be presumed to occur without considering the effect of posterior corneal astigmatism (PCA). The light blue and pink dashed lines and image lines “c” and “d” show the actual refraction occurring at the posterior corneal surface. A Shows overestimation of WTR astigmatism that occurs if PCA is not taken into account. B Shows underestimation of ATR astigmatism that occurs if PCA is not taken into account.
Maximum refractive power of the eye is at the front surface of the cornea because of the significant difference in refractive indices between air and cornea. Keratometers and topographers give measurements of anterior corneal surface and thereby of anterior corneal astigmatism (ACA). However, we know now that despite the low difference in refractive indices of aqueous and stroma, posterior corneal astigmatism (PCA) does affect total corneal astigmatism (TCA), contributing an average of about 0.50 Dioptres (D) of against-therule (ATR) change.
TCA may be roughly calculated from ACA by using simplified Javal’s rule: “TCA=ATR_ACA@180o+ (+0.50@180o)” or “TCA=WTR_ACA@90o+ (-0.50@90o).”
This implies that TCA is generally less in case of with-the-rule (WTR) ACA and therefore using keratometric values alone can result in overestimation of the astigmatism by 0.5-to-0.6D and thereby an overcorrection.
Similarly, TCA is generally more in case of ATR ACA resulting in underestimation by 0.2-to-0.3D and under-correction of astigmatism if treatment is based on ACA alone. According to a 2009 study by Ho et al, PCA on an average caused reduction of TCA by 13.4% and in approximately 30% of eyes, PCA caused a change in TCA by >0.5D or by >10o in meridian from ACA.
For a long time, the reason for suboptimal results after toric IOL implantation was unclear and was attributed to lenticular astigmatism and even to the retina. However, recently, the posterior cornea has been studied in much greater detail. Koch et al’s paper from 2012 that analysed 715 corneas of 435 consecutive patients found that the steep corneal meridian was aligned vertically, between 60 and 120o in 51.9% of eyes for anterior surface and 86.6% of eyes for posterior surface. Since the posterior cornea is a negative lens, however, the vertically steep posterior curvature results in a net positive power in the horizontal direction or an ATR astigmatism.
They also found that with increasing WTR ACA, the PCA can also increase, even up to 1D. However, this is not the case with increasing ATR ACA, where mean PCA remains relatively same. In addition, with increasing age, the anterior cornea tended to change from WTR to ATR, yet this drift was not seen in the posterior cornea. A 2015 study by Hiyashi et al also showed an ATR drift of 0.2-to-0.4D in all age groups, during a 10-year follow-up in both post-cataract surgery as well as no surgery groups, with the drift further continuing over 20 years, as shown in their 2017 follow-up study.
Another interesting study was by Ueno et al, using swept-source OCT, which showed that the cornea is thicker along the vertical than the horizontal meridian, and this could contribute to ATR astigmatism by creating a steeper vertical cornea posteriorly. This difference was found to increase with age, which could partially account for the ATR drift in old age. Another finding was that the superior cornea was thicker than the inferior cornea and could possibly contribute to some higher-order aberrations.
MEASUREMENT OF POSTERIOR CORNEAL ASTIGMATISM
This may be done by newer and better tomographers, such as Scheimpflug imaging, slit scanning, OCT and reflective LED imaging, that allow measurement of the posterior cornea. However, accurate measurement of the posterior corneal curvature is still not possible and this led to the development and popularity of the Baylor nomogram. Another popular option is to use a theoretical approach such as used in the Barrett toric IOL calculator (www.ascrs.org).
BAYLOR NOMOGRAM
This regression approach based on population averages was proposed by Koch et al in their 2013 study to correct overestimation of WTR and underestimation of ATR. The surgically induced astigmatism (SIA- usually between 0.2 and 0.3D for most surgeons) is first factored in, followed by IOL’s spherical power and its position in the eye as these can affect the toricity at corneal plane. The nomogram then corrects for PCA by increasing or decreasing from that IOL power. It also factors in an additional adjustment to leave patients with slight WTR astigmatism to counter the ATR drift that occurs with ageing. These adjustments lead to a change in threshold for implanting toric IOLs to about 1.7D of WTR and 0.8D of ATR ACA after factoring in of SIA.
Many patients with oblique astigmatism may be considered to be midway in the age-related drift from WTR to ATR and these patients should be targeted on or only slightly below measured astigmatism. The toric IOL should therefore be aligned on axis or towards ATR axis and not towards the WTR axis in order to hold good for a longer time during the ATR drift.
BARRETT TORIC CALCULATOR
This incorporates the patient’s PCA and effective lens position (ELP) values rather than using population averages. However, it is based on a theoretical eye and PCA and ELP are predicted rather than measured though recent updates allow input of measured values as well. It uses anterior chamber depth (ACD), axial length, toricity ratio and SIA centroid for its calculations. For calculation of spherical equivalent IOL power, it bases itself on Barrett Universal II formula, where ACD is related to axial length and keratometry and principal plane of refraction of IOL is a variable. The Barrett True K Toric calculator is used in post-refractive surgery eyes.
Other formulae in use for toric IOL calculation include ASSORT calculator, Savini calculator, Holladay IOL consultant software etc.
To conclude, PCA is important for estimating power of the toric IOL to be implanted. IOL with less toricity needs to be chosen when correcting WTR astigmatism and conversely, more toricity when correcting ATR astigmatism.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India and can be reached at dr_soosanj@hotmail.com
Tags: toric IOLs
Latest Articles
Overcoming Barriers to Presbyopic IOL Uptake
Improving technology, patient and doctor awareness, and reimbursement are keys.
Training in the Digital Era
AI-powered, cloud-based system can effectively improve traineeship, save time, and increase performance.
Treating Myopia, Inside and Outside
Lifestyle changes and ophthalmic interventions play a role in treating paediatric myopia.
The Promises and Pitfalls of AI
While AI shows potential in healthcare, experts agree it requires bias mitigation and human oversight.
Visual Rehabilitation for Keratoconus
Concepts regarding best techniques shift based on learnings from longer follow-up.
Discovering Prodygy and Nirvana
New gene-agnostic treatments for inheritable retinal disease.
Cataract Surgery in Eyes with Corneal Disease
Applying information from preoperative diagnostics guides surgical planning.
Supplement: Integrating Presbyopia-Correction into the Everyday Cataract Practice
ESCRS Research Projects Make a Difference
EPICAT study continues tradition of practice-changing clinical studies.