Complications of cataract and refractive surgery
Any number of complications can occur in or after surgery, and it's important to keep things in perspective.

Soosan Jacob
Published: Friday, June 5, 2020
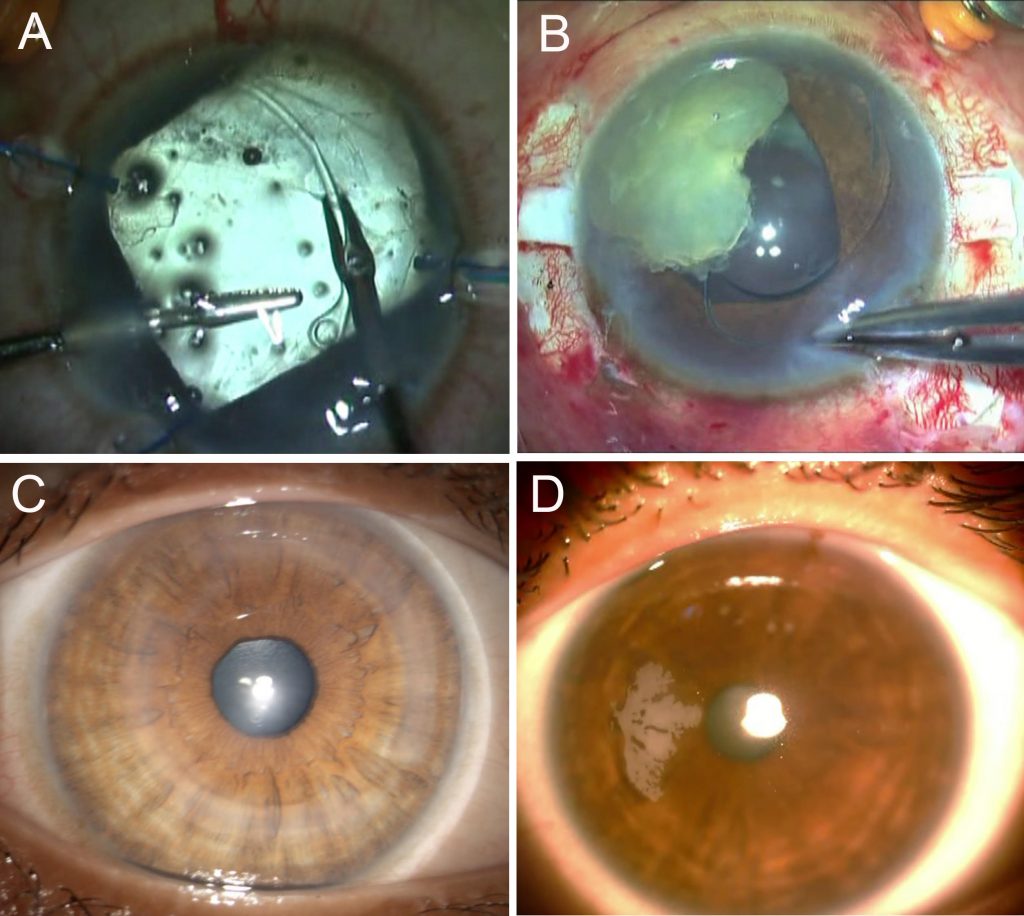 A: Capsular tension ring implantation in subluxated cataract; B: IOL scaffold for PCR;
C: CAIRS (Corneal Allogenic Intrastromal ring Segment) for corneal ectasia; D: Post-SMILE epithelial ingrowth
As precision surgeons aiming for excellent unaided distance and near visual acuity, we feel uncomfortable hearing the word “complications”. However, the best way to manage complications is to be prepared. In this article, I will try and pen my thoughts on preventing/ managing complications in a concise but obviously not comprehensive manner.
CATARACT SURGERY COMPLICATIONS:
I like to think of complications as those that I am terrified of, those that worry me a lot and others.
TERRIFIED OF
Endophthalmitis and infections: This terrifies each of us because of the potential of even best planned surgeries going wrong. The cause can sometimes be outside our control, such as contaminated solutions/eye drops that are labelled ‘sterile’ or even patient factors such as poor hygiene and postoperative care. Key in these situations is of course early identification and referral to the vitreoretinal surgeon. Highly virulent organisms such as Pseudomonas can take their toll despite timely intervention.
Simultaneous with treatment, it is important to keep an open channel of communication with the patient, to not lose trust and to help them navigate this unexpected outcome and territory. Especially with the present trend to consider the physician as a service provider, it becomes imperative to educate lay population, media as well as governmental agencies about the multi-factorial causation for endophthalmitis, especially in cluster outbreaks.
Supra-choroidal and expulsive haemorrhage: Though rarer in cataract surgery, this can still occur and has the potential to turn rapidly ugly. Shallowing of the anterior chamber (AC), a firm eye, loss of red reflex and bulging of the posterior capsule should be recognised immediately. Your first aim should be to withdraw instruments and suture all incisions closed. The AC may be deepened with viscoelastic if possible. Prolapsed iris may need to be excised and any further surgery should be deferred. Surgical drainage via sclerotomy is not advisable, as it results in loss of tamponading effect and further bleeding.
WORRIES ME A LOT
Posterior capsular rent (PCR): Most important of course here, is not to pull out the phaco or I/A probe abruptly, as this can result in extension of the tear and vitreous prolapse. Viscodispersive viscoelastic is injected under the remaining pieces and over the PCR and the probe is gently removed. Key here for me, is the stage at which PCR occurrs.
If entire/ large part of a hard nucleus is present, I prefer to convert to manual small-incision cataract extraction, which is self-sealing while allowing safe removal of nucleus.
If it is only a soft cataract or a small fragment left behind, I bring it over the iris and then perform an IOL scaffold technique by preplacing a three-piece IOL into the sulcus with optic capture and then emulsifying the nucleus. This prevents fragments from dropping into the vitreous. The cortex, however, should be removed before implanting the IOL. I do this with a vitrector probe via a pars plana approach, alternating between cut and aspirate modes to avoid vitreous traction while allowing easy cortex aspiration.
Persistent corneal oedema: Preoperative specular count helps identify early Fuchs’ dystrophy. Viscodispersive viscoelastic, in-the-bag chop, low energy usage, torsional ultrasound all help decrease corneal damage. In advanced cases, phaco may be combined with endothelial keratoplasty (EK).
If corneal oedema is seen postoperatively in a patient with normal preoperative endothelial count, I do an ASOCT to rule out Descemet’s detachment (DD), which if present can be easily bubbled. Bullous DD, which I had described as a type of DD, may occur during stromal hydration of side port. This may not respond to air/long-acting gas alone and I do Relaxing Descemetotomy to drain trapped fluid.
In recalcitrant oedema, I prefer doing pre-Descemet’s EK using three techniques also described by me – endoilluminator and air pump-assisted techniques as well as host Descemetic scaffolding, which make surgery easier, repeatable and decrease chances of graft detachment.
Retinal complications: These are worrisome, especially a retinal detachment. Chances increase in high myopes and complicated surgeries. A retinal surgeon should be consulted immediately. Postoperative cystoid macular oedema may also occur and prophylactic topical NSAIDs are helpful to prevent it. This should be treated aggressively if present.
Malpositioned IOL: An IOL that is not properly placed at time of surgery or that gets dislocated due to various reasons worries me since it requires a second intervention. Eyes with deficient anterior/posterior capsular support need stable IOL fixation during primary surgery in the form of iris or scleral fixation or even (though not my personal preference), an ACIOL. A single-piece acrylic IOL placed with haptic in sulcus can cause uveitis-glaucoma-hyphema syndrome and needs to be repositioned. Late postoperative dislocations can occur because of suture degradation and progressive zonulopathies.
OTHER COMPLICATIONS
Refractive error: In patients who opt for premium IOL with the aim of decreasing spectacle dependence, I generally find that having done a proper preoperative counselling sets expectations straight for small postoperative refractive errors. However, large refractive surprises can be upsetting and may entail either cornea-based refractive surgery, piggyback IOL, IOL exchange or sometimes just an IOL rotation in case of toric IOLs.
Dysphotopsias: Positive dysphotopsias such as glare, haloes etc occur secondary to poor optics of the eye (increased higher-order aberrations, large-angle kappa) or the IOL (diffractive IOLs, truncated edges, high refractive index IOLs) and can be treated by pharmacological pupillary constriction. Unresponsive and persistent cases may need an IOL exchange. Negative dysphotopsias occur because of a gap between rays refracted by IOL and those passing without going through IOL. Negative dysphtopsias are managed by special glasses that block light entering from the side. Just waiting for capsular opacification to cause light scatter on to the dark area of the retina may also work. Surgical options include removing nasal overlapping capsule, reverse optic capture, orienting optic haptic junction to horizontal meridian or exchanging with a three-piece silicone IOL. Pupillary constriction can however worsen it.
Other complications such as postoperative glaucoma, inflammation, posterior capsular opacities etc may occur and can generally be handled well with appropriate and timely treatment. Complications in special situations such as IOL opacification following intracameral air in hydrophilic IOLs, corneal melts in patients with rheumatoid arthritis, severe postoperative inflammation in uveitic patients etc need special evaluation and planning pre- and postoperatively.
REFRACTIVE SURGERY COMPLICATIONS
Refractive cataract surgery complications are already discussed above. Other forms of refractive surgery can also have complications, though the rate is generally low.
PHAKIC IOLs (PIOLs)
PIOLs have distinct complications depending on whether they are AC or posterior chamber (PC) PIOLs. The vaulting of a PCPIOL is important and a low vault can cause cataract while an excessive vault can cause shallow AC, angle closure and increased IOP. ACPIOLs can cause endothelial decompensation, glaucoma and pupillary abnormalities/ distortion.
My personal preference is to place a PCPIOL as it is easier for me and for the patient if I have to treat a potential cataract formation than a potential endothelial decompensation. Others surgeons, however, have their own preference depending on their experience. Since these are all intraocular surgeries, they do carry the risk of complications such as uveitis, retinal detachment, endophthalmitis etc. I give prime importance to performing a thorough dilated retinal examination pre-operatively to avoid potential retinal detachments and avoid operating on very high-risk patients.
CORNEA-BASED REFRACTIVE SURGERY COMPLICATIONS
TERRIFIES ME
Infections: As always, postoperative infections always terrify me. Luckily, however, the rate of infections post refractive surgery is very low and proper precautions continue to maintain this so. Post-PRK infections may occur secondary to epithelial defect and use of contact lenses. Post-LASIK infections are unlike usual corneal infections and proper management is a must. Interface involvement, delayed presentation, steroid usage, atypical and resistant organisms, inadequate drug penetration, indolent course and slow response to therapy are seen.
WORRIES ME A LOT
Flap complications: Buttonholes, free caps, perforations, decentred flap, amputated flap, partial flap all occur more often with microkeratome but also do occur with femtosecond laser. Buttonholes are managed by deferred surface ablation, whereas free caps can undergo excimer ablation with careful flap replacement. Partial flap with microkeratome is deferred for later treatment whereas if with femtosecond, the cut can be resumed. Small-incision lenticule extraction (SMILE®) can have complications with lenticule creation, dissection and extraction.
Ectasia: Preoperative evaluation and risk scoring is important. Sometimes a patient who has no risk factor on tomography may still present with ectasia. Preoperative biomechanical screening may be useful in the form of Corvis Biomechanical index and Tomographic Biomechanical index. Ectasia should be treated early with cross-linking to minimise damage to vision as well as avoiding more invasive surgeries such as deep anterior lamellar keratoplasty.
In advanced cases, intra-stromal corneal ring segments such as Intacs and CAIRS (Corneal Allogenic Intrastromal Ring Segments) can be used simultaneous with CXL to improve uncorrected visual acuity.
Aberrated optics: This may occur secondary to central island, decentred ablation, irregular astigmatism and even early post-LASIK ectasia. Patients have glare, haloes and decreased uncorrected and best-corrected visual acuity, often worse at night. Tomographic evaluation is needed to rule out ectasia. I then generally give some time for epithelial remodelling and also use brimonidine eye drops for pupillary constriction to try and relieve symptoms non-surgically.
Unresponsive and persistent cases may respond to rigid gas permeable contact lenses or topography-guided therapeutic refractive surgery. In SMILE, partially retained lenticule can cause irregular astigmatism and symptoms. Fourier domain OCT and diluted IVTA can be used to delineate the retained fragment and remove it. In Epi-LASIK, stromal injury from blade can cause irregular astigmatism and in case of an uneven bed, ablation should be postponed.
Dysphotoptic symptoms:
Patients may complain of glare, haloes, ghosting and night vision abnormalities. These are more common with larger corrections, smaller optic zone, aberrated optics (see above) and larger pupil size (more important with older laser technology). Transient light sensitivity occurs in some patients but generally responds to treatment.
Epithelial ingrowth, Striae, Diffuse Lamellar keratitis (DLK), Interface debris: These complications can generally be addressed with good resolution. I leave subtle peripheral striae and inactive, peripheral epithelial ingrowth alone but symptomatic ones need intervention. DLK always needs to be treated aggressively with steroids and in more advanced cases with flap lift and wash.
OTHER COMPLICATIONS
I always make sure that refractive expectations are set right by proper counselling. I take care to explain that though refractive surgery in its current form gives excellent results, both efficacy and safety-wise, it cannot guarantee spectacle independency for all activities for every single patient. I have rarely seen situations where an otherwise happy 20/20 patient becomes concerned on seeing +/-0.25 to 0.5DS spherical equivalent come up on autorefractor reading, as they expect it to come to a perfect zero.
Consent and patient counselling should include complications such as dry eye and the possibility of some residual refractive error. Over-corrections and under-corrections may occur and are generally treatable after refractive stabilization. Aggressive topical steroids can be used for under-corrections. Deep surface ablations can be prone to haze/regression and Mitomicin-C is used intra-operatively.
To conclude, complications are an inevitable part of every surgeon’s life and these should be dealt with properly either by the surgeon or through specialist referral.
* Dr Soosan Jacob is Director and Chief of Dr Agarwal's Refractive and Cornea Foundation at Dr Agarwal's Eye Hospital, Chennai, India and can be reached at dr_soosanj@hotmail.com
A: Capsular tension ring implantation in subluxated cataract; B: IOL scaffold for PCR;
C: CAIRS (Corneal Allogenic Intrastromal ring Segment) for corneal ectasia; D: Post-SMILE epithelial ingrowth
As precision surgeons aiming for excellent unaided distance and near visual acuity, we feel uncomfortable hearing the word “complications”. However, the best way to manage complications is to be prepared. In this article, I will try and pen my thoughts on preventing/ managing complications in a concise but obviously not comprehensive manner.
CATARACT SURGERY COMPLICATIONS:
I like to think of complications as those that I am terrified of, those that worry me a lot and others.
TERRIFIED OF
Endophthalmitis and infections: This terrifies each of us because of the potential of even best planned surgeries going wrong. The cause can sometimes be outside our control, such as contaminated solutions/eye drops that are labelled ‘sterile’ or even patient factors such as poor hygiene and postoperative care. Key in these situations is of course early identification and referral to the vitreoretinal surgeon. Highly virulent organisms such as Pseudomonas can take their toll despite timely intervention.
Simultaneous with treatment, it is important to keep an open channel of communication with the patient, to not lose trust and to help them navigate this unexpected outcome and territory. Especially with the present trend to consider the physician as a service provider, it becomes imperative to educate lay population, media as well as governmental agencies about the multi-factorial causation for endophthalmitis, especially in cluster outbreaks.
Supra-choroidal and expulsive haemorrhage: Though rarer in cataract surgery, this can still occur and has the potential to turn rapidly ugly. Shallowing of the anterior chamber (AC), a firm eye, loss of red reflex and bulging of the posterior capsule should be recognised immediately. Your first aim should be to withdraw instruments and suture all incisions closed. The AC may be deepened with viscoelastic if possible. Prolapsed iris may need to be excised and any further surgery should be deferred. Surgical drainage via sclerotomy is not advisable, as it results in loss of tamponading effect and further bleeding.
WORRIES ME A LOT
Posterior capsular rent (PCR): Most important of course here, is not to pull out the phaco or I/A probe abruptly, as this can result in extension of the tear and vitreous prolapse. Viscodispersive viscoelastic is injected under the remaining pieces and over the PCR and the probe is gently removed. Key here for me, is the stage at which PCR occurrs.
If entire/ large part of a hard nucleus is present, I prefer to convert to manual small-incision cataract extraction, which is self-sealing while allowing safe removal of nucleus.
If it is only a soft cataract or a small fragment left behind, I bring it over the iris and then perform an IOL scaffold technique by preplacing a three-piece IOL into the sulcus with optic capture and then emulsifying the nucleus. This prevents fragments from dropping into the vitreous. The cortex, however, should be removed before implanting the IOL. I do this with a vitrector probe via a pars plana approach, alternating between cut and aspirate modes to avoid vitreous traction while allowing easy cortex aspiration.
Persistent corneal oedema: Preoperative specular count helps identify early Fuchs’ dystrophy. Viscodispersive viscoelastic, in-the-bag chop, low energy usage, torsional ultrasound all help decrease corneal damage. In advanced cases, phaco may be combined with endothelial keratoplasty (EK).
If corneal oedema is seen postoperatively in a patient with normal preoperative endothelial count, I do an ASOCT to rule out Descemet’s detachment (DD), which if present can be easily bubbled. Bullous DD, which I had described as a type of DD, may occur during stromal hydration of side port. This may not respond to air/long-acting gas alone and I do Relaxing Descemetotomy to drain trapped fluid.
In recalcitrant oedema, I prefer doing pre-Descemet’s EK using three techniques also described by me – endoilluminator and air pump-assisted techniques as well as host Descemetic scaffolding, which make surgery easier, repeatable and decrease chances of graft detachment.
Retinal complications: These are worrisome, especially a retinal detachment. Chances increase in high myopes and complicated surgeries. A retinal surgeon should be consulted immediately. Postoperative cystoid macular oedema may also occur and prophylactic topical NSAIDs are helpful to prevent it. This should be treated aggressively if present.
Malpositioned IOL: An IOL that is not properly placed at time of surgery or that gets dislocated due to various reasons worries me since it requires a second intervention. Eyes with deficient anterior/posterior capsular support need stable IOL fixation during primary surgery in the form of iris or scleral fixation or even (though not my personal preference), an ACIOL. A single-piece acrylic IOL placed with haptic in sulcus can cause uveitis-glaucoma-hyphema syndrome and needs to be repositioned. Late postoperative dislocations can occur because of suture degradation and progressive zonulopathies.
OTHER COMPLICATIONS
Refractive error: In patients who opt for premium IOL with the aim of decreasing spectacle dependence, I generally find that having done a proper preoperative counselling sets expectations straight for small postoperative refractive errors. However, large refractive surprises can be upsetting and may entail either cornea-based refractive surgery, piggyback IOL, IOL exchange or sometimes just an IOL rotation in case of toric IOLs.
Dysphotopsias: Positive dysphotopsias such as glare, haloes etc occur secondary to poor optics of the eye (increased higher-order aberrations, large-angle kappa) or the IOL (diffractive IOLs, truncated edges, high refractive index IOLs) and can be treated by pharmacological pupillary constriction. Unresponsive and persistent cases may need an IOL exchange. Negative dysphotopsias occur because of a gap between rays refracted by IOL and those passing without going through IOL. Negative dysphtopsias are managed by special glasses that block light entering from the side. Just waiting for capsular opacification to cause light scatter on to the dark area of the retina may also work. Surgical options include removing nasal overlapping capsule, reverse optic capture, orienting optic haptic junction to horizontal meridian or exchanging with a three-piece silicone IOL. Pupillary constriction can however worsen it.
Other complications such as postoperative glaucoma, inflammation, posterior capsular opacities etc may occur and can generally be handled well with appropriate and timely treatment. Complications in special situations such as IOL opacification following intracameral air in hydrophilic IOLs, corneal melts in patients with rheumatoid arthritis, severe postoperative inflammation in uveitic patients etc need special evaluation and planning pre- and postoperatively.
REFRACTIVE SURGERY COMPLICATIONS
Refractive cataract surgery complications are already discussed above. Other forms of refractive surgery can also have complications, though the rate is generally low.
PHAKIC IOLs (PIOLs)
PIOLs have distinct complications depending on whether they are AC or posterior chamber (PC) PIOLs. The vaulting of a PCPIOL is important and a low vault can cause cataract while an excessive vault can cause shallow AC, angle closure and increased IOP. ACPIOLs can cause endothelial decompensation, glaucoma and pupillary abnormalities/ distortion.
My personal preference is to place a PCPIOL as it is easier for me and for the patient if I have to treat a potential cataract formation than a potential endothelial decompensation. Others surgeons, however, have their own preference depending on their experience. Since these are all intraocular surgeries, they do carry the risk of complications such as uveitis, retinal detachment, endophthalmitis etc. I give prime importance to performing a thorough dilated retinal examination pre-operatively to avoid potential retinal detachments and avoid operating on very high-risk patients.
CORNEA-BASED REFRACTIVE SURGERY COMPLICATIONS
TERRIFIES ME
Infections: As always, postoperative infections always terrify me. Luckily, however, the rate of infections post refractive surgery is very low and proper precautions continue to maintain this so. Post-PRK infections may occur secondary to epithelial defect and use of contact lenses. Post-LASIK infections are unlike usual corneal infections and proper management is a must. Interface involvement, delayed presentation, steroid usage, atypical and resistant organisms, inadequate drug penetration, indolent course and slow response to therapy are seen.
WORRIES ME A LOT
Flap complications: Buttonholes, free caps, perforations, decentred flap, amputated flap, partial flap all occur more often with microkeratome but also do occur with femtosecond laser. Buttonholes are managed by deferred surface ablation, whereas free caps can undergo excimer ablation with careful flap replacement. Partial flap with microkeratome is deferred for later treatment whereas if with femtosecond, the cut can be resumed. Small-incision lenticule extraction (SMILE®) can have complications with lenticule creation, dissection and extraction.
Ectasia: Preoperative evaluation and risk scoring is important. Sometimes a patient who has no risk factor on tomography may still present with ectasia. Preoperative biomechanical screening may be useful in the form of Corvis Biomechanical index and Tomographic Biomechanical index. Ectasia should be treated early with cross-linking to minimise damage to vision as well as avoiding more invasive surgeries such as deep anterior lamellar keratoplasty.
In advanced cases, intra-stromal corneal ring segments such as Intacs and CAIRS (Corneal Allogenic Intrastromal Ring Segments) can be used simultaneous with CXL to improve uncorrected visual acuity.
Aberrated optics: This may occur secondary to central island, decentred ablation, irregular astigmatism and even early post-LASIK ectasia. Patients have glare, haloes and decreased uncorrected and best-corrected visual acuity, often worse at night. Tomographic evaluation is needed to rule out ectasia. I then generally give some time for epithelial remodelling and also use brimonidine eye drops for pupillary constriction to try and relieve symptoms non-surgically.
Unresponsive and persistent cases may respond to rigid gas permeable contact lenses or topography-guided therapeutic refractive surgery. In SMILE, partially retained lenticule can cause irregular astigmatism and symptoms. Fourier domain OCT and diluted IVTA can be used to delineate the retained fragment and remove it. In Epi-LASIK, stromal injury from blade can cause irregular astigmatism and in case of an uneven bed, ablation should be postponed.
Dysphotoptic symptoms:
Patients may complain of glare, haloes, ghosting and night vision abnormalities. These are more common with larger corrections, smaller optic zone, aberrated optics (see above) and larger pupil size (more important with older laser technology). Transient light sensitivity occurs in some patients but generally responds to treatment.
Epithelial ingrowth, Striae, Diffuse Lamellar keratitis (DLK), Interface debris: These complications can generally be addressed with good resolution. I leave subtle peripheral striae and inactive, peripheral epithelial ingrowth alone but symptomatic ones need intervention. DLK always needs to be treated aggressively with steroids and in more advanced cases with flap lift and wash.
OTHER COMPLICATIONS
I always make sure that refractive expectations are set right by proper counselling. I take care to explain that though refractive surgery in its current form gives excellent results, both efficacy and safety-wise, it cannot guarantee spectacle independency for all activities for every single patient. I have rarely seen situations where an otherwise happy 20/20 patient becomes concerned on seeing +/-0.25 to 0.5DS spherical equivalent come up on autorefractor reading, as they expect it to come to a perfect zero.
Consent and patient counselling should include complications such as dry eye and the possibility of some residual refractive error. Over-corrections and under-corrections may occur and are generally treatable after refractive stabilization. Aggressive topical steroids can be used for under-corrections. Deep surface ablations can be prone to haze/regression and Mitomicin-C is used intra-operatively.
To conclude, complications are an inevitable part of every surgeon’s life and these should be dealt with properly either by the surgeon or through specialist referral.
* Dr Soosan Jacob is Director and Chief of Dr Agarwal's Refractive and Cornea Foundation at Dr Agarwal's Eye Hospital, Chennai, India and can be reached at dr_soosanj@hotmail.com
Tags: cataract and refractive complictions
Latest Articles
Making Female Leadership More than a Moment
A remarkable global confluence of women in key positions.
ESCRS Talks Technology at AAO
Europe adopts technological advances, US still waiting for lenses and lasers.
Sorting Out Simultaneous Vision IOLs
The ESCRS Eye Journal Club discuss a new landmark paper on IOL classification and the need for harmonisation of terminology for presbyopic IOLs.
Big Advantages to Small-Aperture IOLs
Small-aperture IOLs offer superior image quality with increased range of focus.
Prioritising Self-Care
Benefits of maintaining physical, emotional, and mental health extend beyond the personal sphere.
Valuing Clinical Trial Design
How inclusivity and diversity can enhance scientific accuracy in research.
Knowing Iris Repair: Using Iridodiathermy in Iris Surgery
Prepare for decentred pupils and uneven irides in multiple situations.
Neuroprotectant Treatment for MacTel Type 2
Intravitreal implant releasing ciliary neurotrophic factor found safe and effective in pivotal trials.