Attaining Excellence in IOL Power Calculations
Dermot McGrath reports

Dermot McGrath
Published: Tuesday, August 31, 2021
Although perfection is not a realistic goal, excellence in refractive outcomes is certainly achievable for the majority of patients undergoing cataract surgery today, according to Adi Abulafia MD.
“Perfection is not attainable, but if we chase perfection, we can catch excellence,” Dr Abulafia said in his keynote address at the online annual meeting of the French Implant and Refractive Surgery Association (SAFIR).
In a wide-ranging lecture, Dr Abulafia—Director of Cataract Services, Ophthalmology Department, Shaare Zedek Medical Centre, Jerusalem, Israel—focused on the remaining challenges towards attaining optimal refractive outcomes for cataract patients.
“Even with all the advances in technology and calculation formulas over the past decade, we are still hovering at a figure of about 80% of patients achieving within 0.50D of their target refraction. That means one out of every five patients will be off target by more than 0.50D, so there is clearly plenty of scope for improvement,” he said.
Dr Abulafia noted five key areas worth highlighting in the quest for better outcomes: accurate preoperative measurements, optimised IOL power calculations, reduced postoperative refractive astigmatism, personalised refraction according to patient needs, and systematic tracking of refractive outcomes.
AXIAL LENGTH
In terms of preoperative biometry, Dr Abulafia said axial length measurements are no longer a major source of inaccuracy, thanks to advanced technology such as swept-source OCT.
“With swept-source OCT, we can maintain a high level of accuracy even in posterior subcapsular and dense cataracts. It makes the use of ultrasound measurements redundant—except perhaps for very dense and mature cataracts,” he said.
It also remains challenging to achieve consistently accurate and reliable measurements for total corneal power, he added.
“Many of our biometry devices measure the anterior corneal curvature in limited zones and extrapolate posterior corneal curvature based on population average-fixed ratios to calculate the estimated total cornea power. While extrapolating the posterior corneal power by a fixed ratio can induce variability in normal corneas, the effect is even more pronounced in atypical corneas such as post-refractive surgery or keratoconus. This will also lead to errors in toric IOL calculations since we are ignoring the posterior corneal astigmatism,” he explained.
Although technologies such as Scheimpflug devices and swept-source OCT are capable of directly measuring the posterior cornea, Dr Abulafia said the accuracy is still far from optimal.
“The small difference in refractive indices between posterior cornea and aqueous makes it a tough surface to identify and quantify,” he said. “There is also no gold standard to validate our measurements. However, a clear advantage of most of the new measuring devices is we can look at raw data to evaluate the actual quality of our measurements to decide whether they are good enough or not.” Eyes with ocular surface disorders such as dry eye, corneal dystrophies, and pterygia, he added, need to be treated first, then remeasured.
MACULAR OCT
Dr Abulafia also suggested introducing macular OCT scans as a routine part of the preoperative work-up.
“In a recent study, we found routine macular OCT scans in cataract patients can help identify macular disease that might be missed or underestimated by standard preoperative examination and can significantly improve patients’ management,” he said.
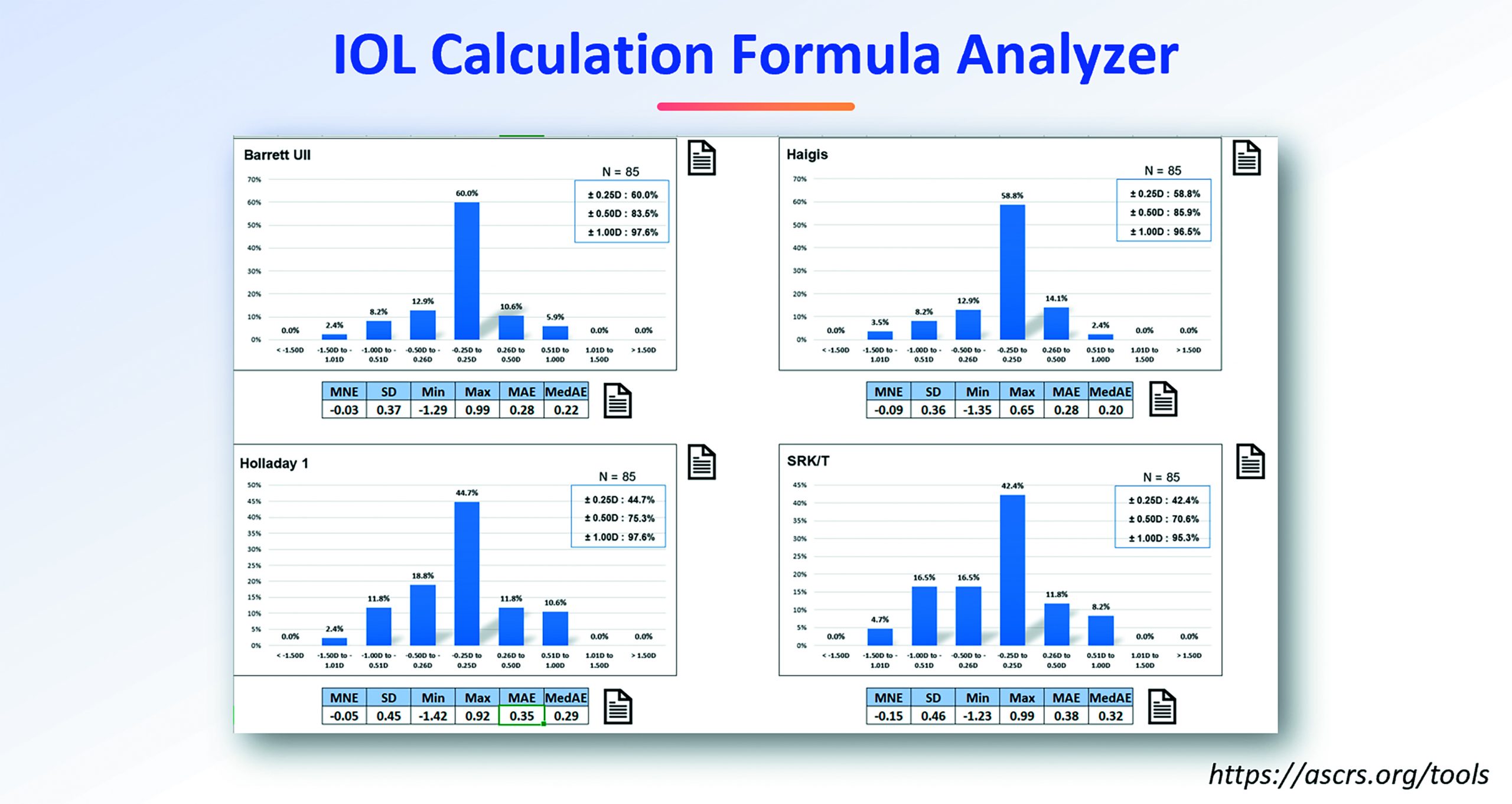
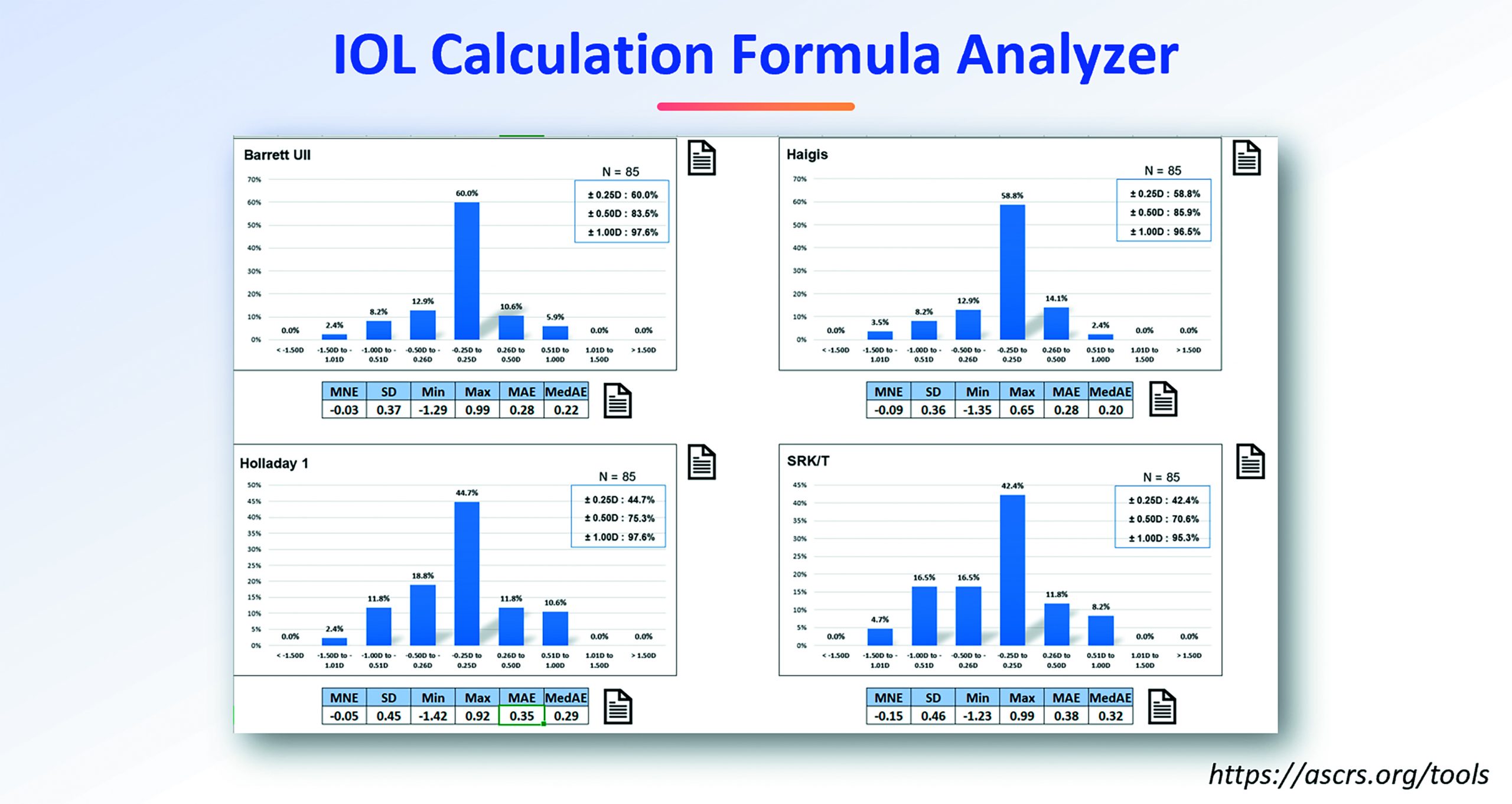
To optimise IOL power calculations, Dr Abulafia advised surgeons to use more recent formulas, drawing on newer
“Perfection is not attainable, but if we chase perfection, we can catch excellence.”
technologies such as paraxial ray tracing, internal sophisticated algorithms, and artificial intelligence (AI) for higher prediction accuracy across a wide range of IOL powers.
“And remember, no formula is perfect, so it is always advisable to compare several formulas before choosing the desired IOL power,” he said.
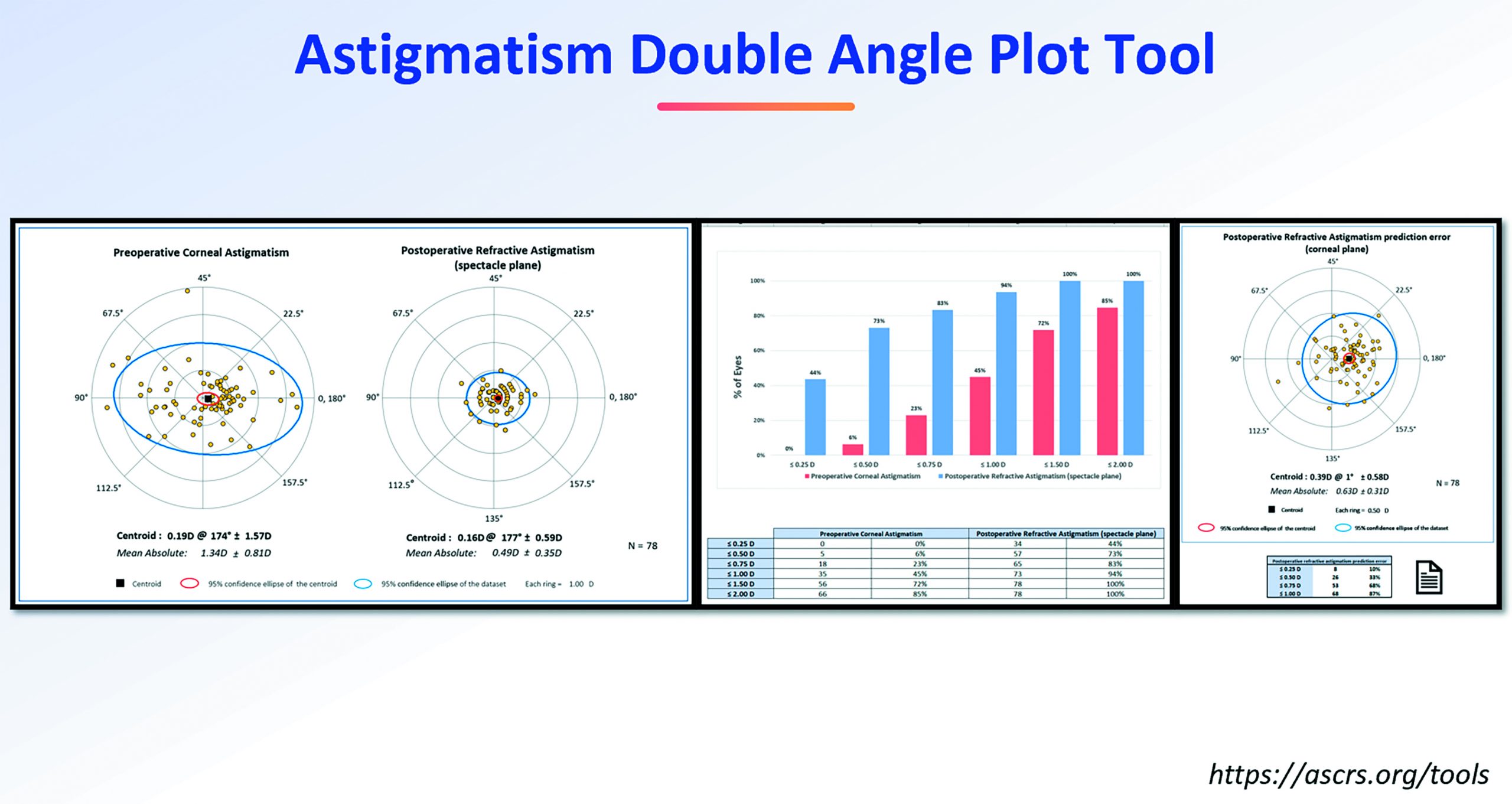
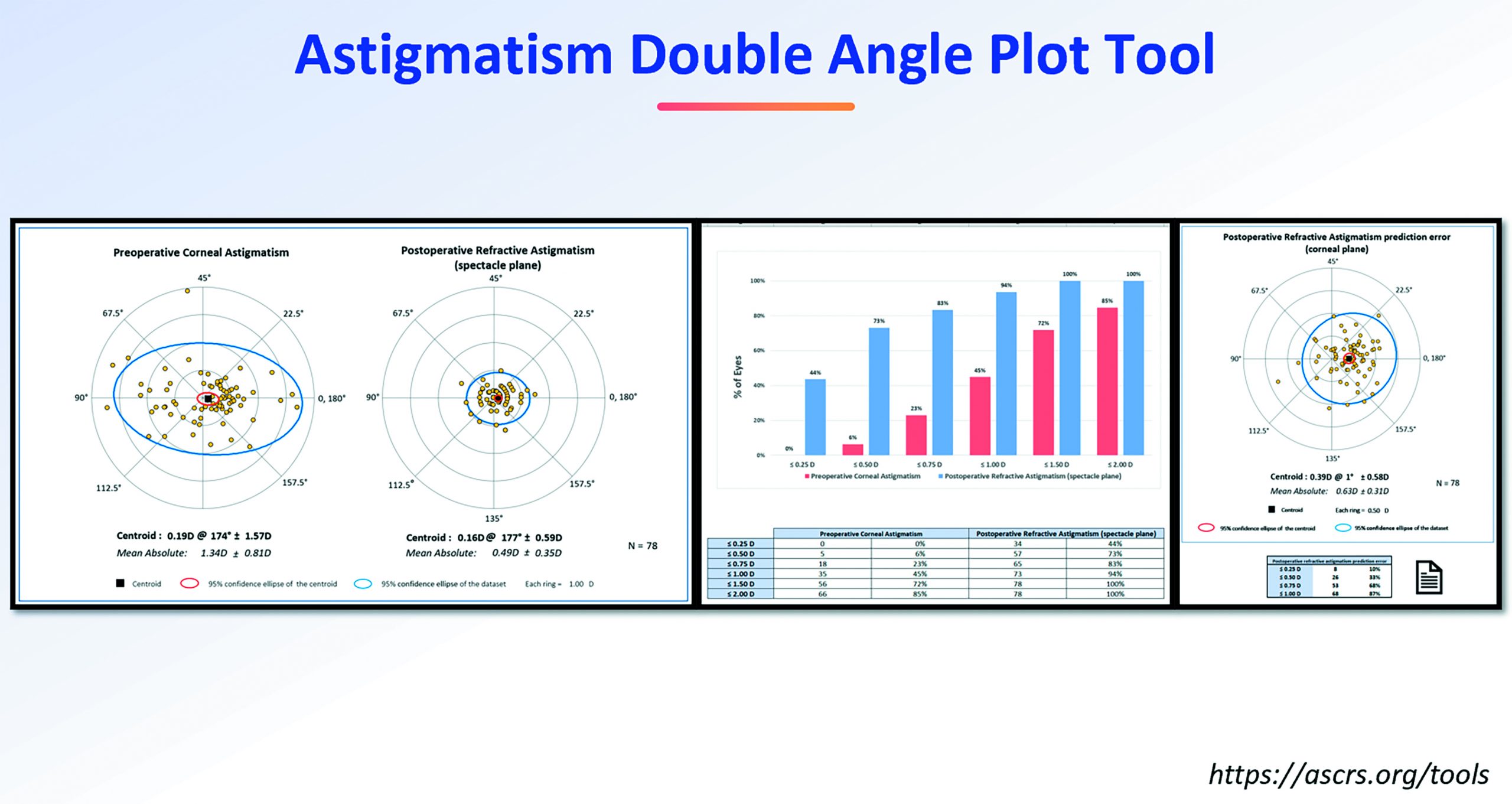
Nailing spherical equivalent (SE) refraction is just one step in the process. Another important challenge is reducing post-op refractive astigmatism.
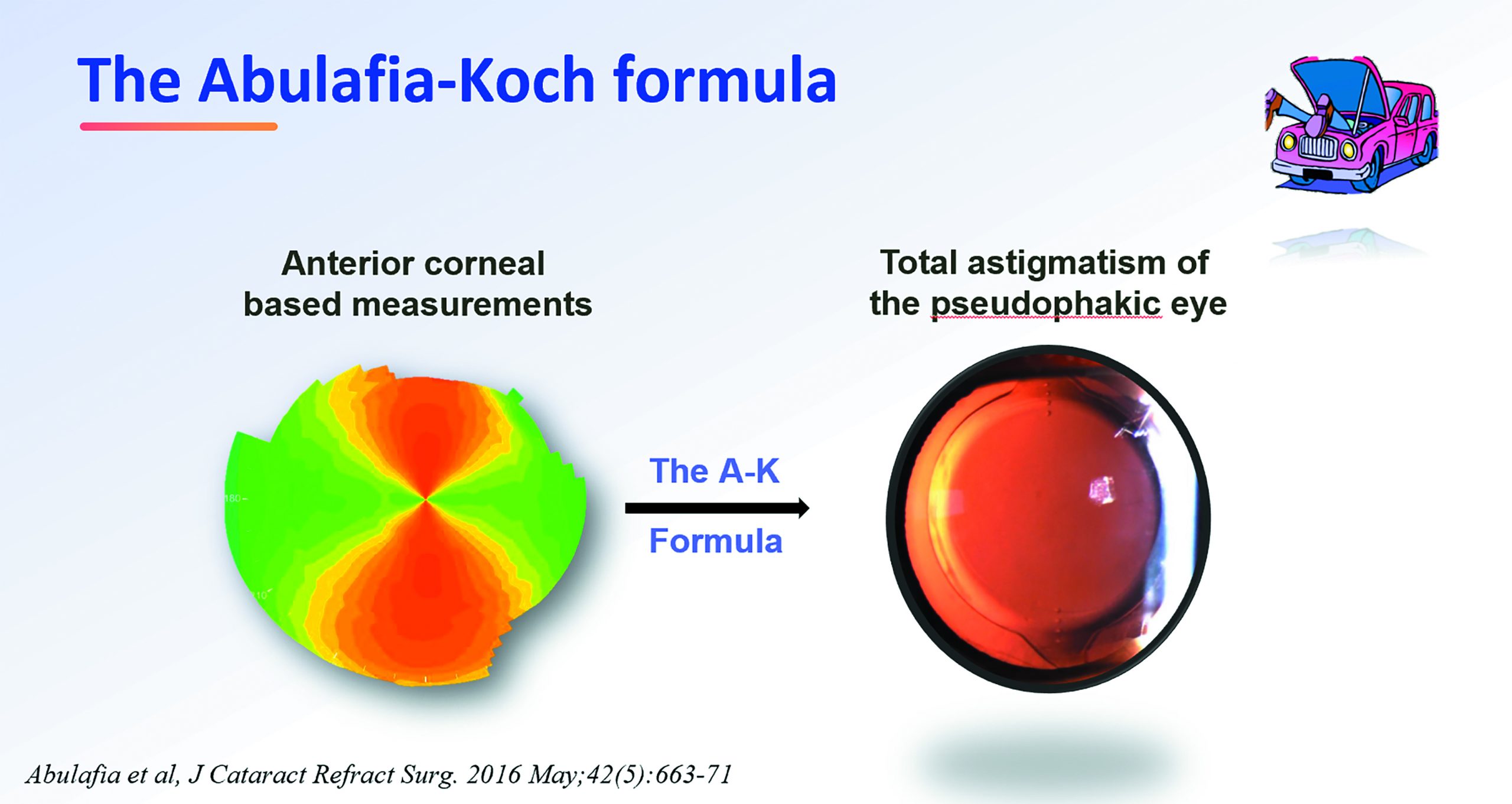
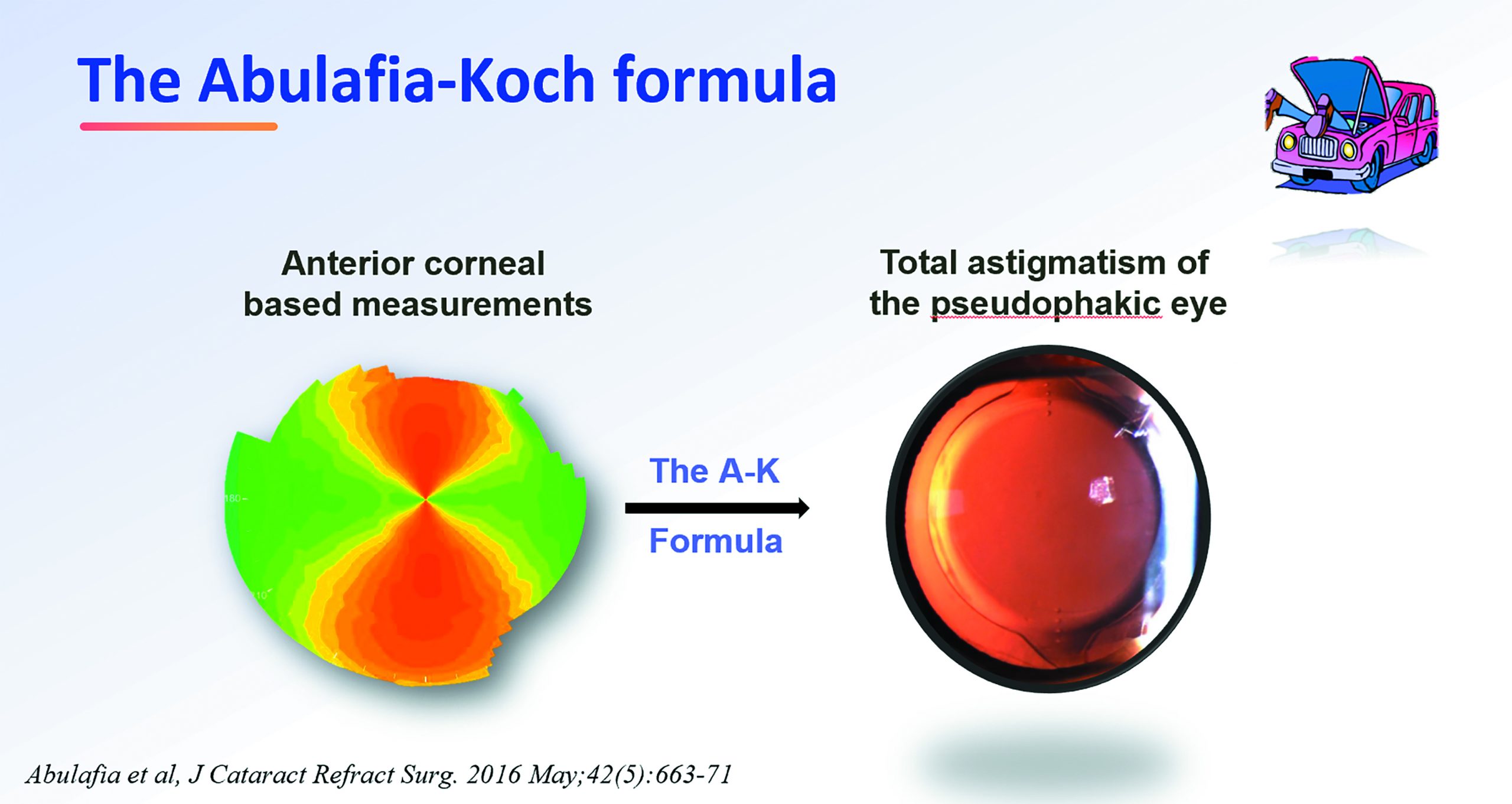
“It is better to use predicted postoperative residual astigmatism as a reference and use several measuring devices where possible. We also need to account for posterior corneal astigmatism and other factors, such as IOL tilt, in our calculations. For this, we can use regression formulas, such as the Abulafia-Koch formula, to compensate for the differences between anterior corneal-based measurements and post-op refraction and improve our outcomes with toric IOLs,” he said.
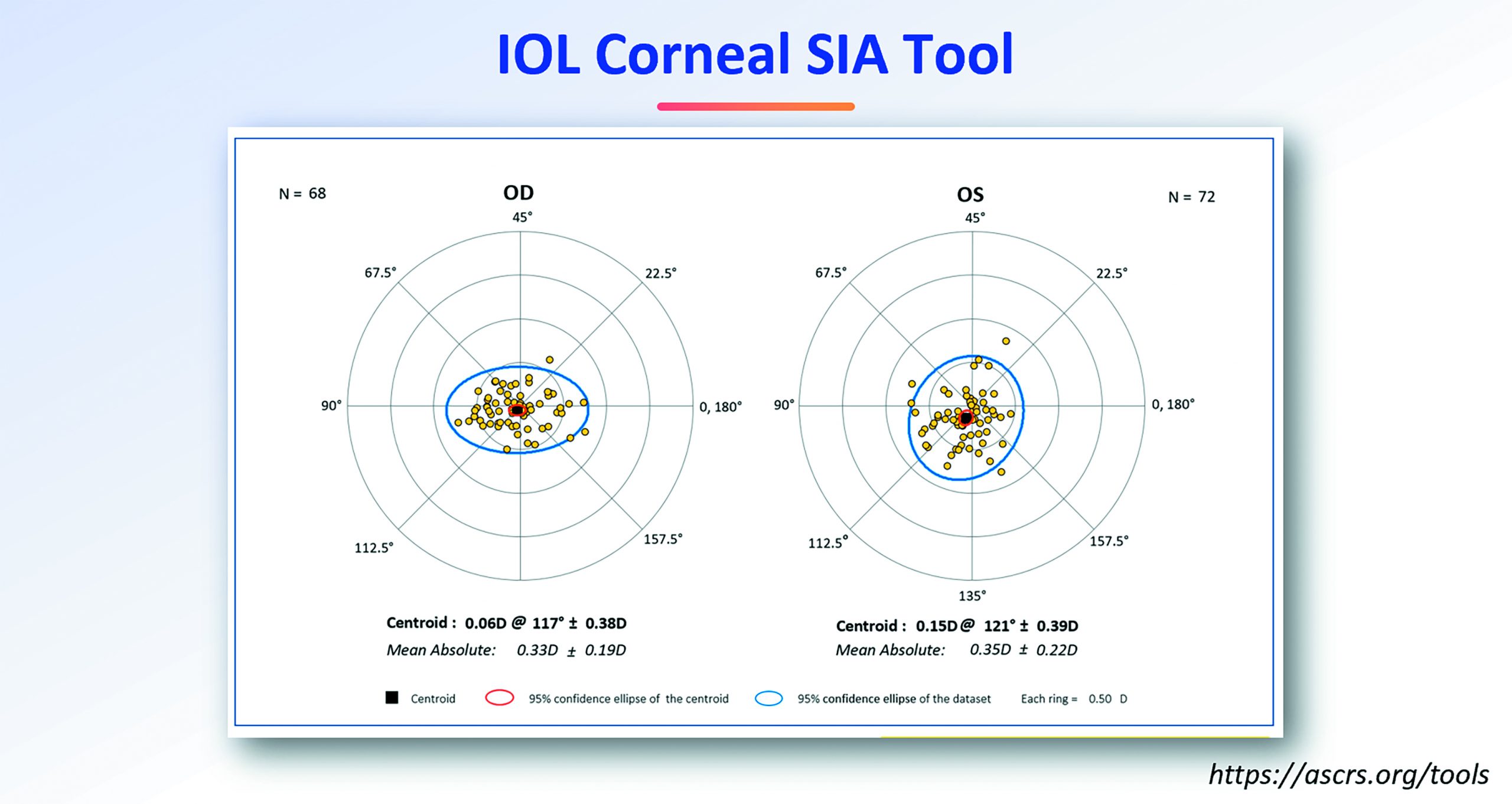
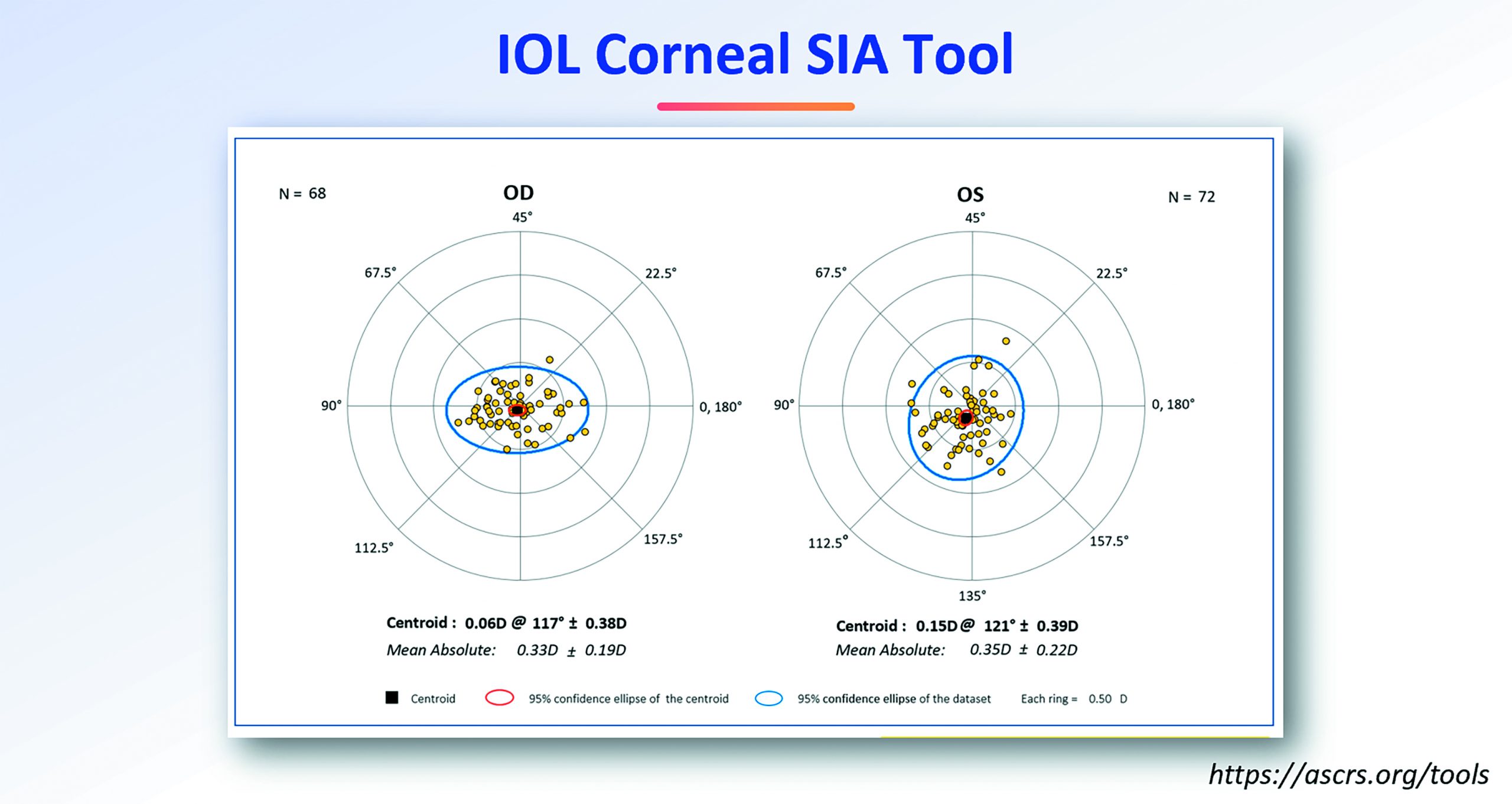
Establishing individual values for surgically induced astigmatism (SIA) can also improve outcomes, he explained.
“This can be a tedious process, and it is not always feasible in some clinical settings. A reasonable compromise would be to use consistent corneal incisions with a low corneal SIA value somewhere between 0.0D and 0.20D,” he said.
The importance of chair time and understanding the patient’s refractive needs in terms of their profession and lifestyle should also not be underestimated.
“We need to tailor the target refraction to our patients’ needs. Hitting the surgeon’s desired refraction can be a complete failure if it is not aligned with their requirements,” he said.
Finally, Dr Abulafia underscored the need to track refractive outcomes.
“This is perhaps the most tedious task of all, but never tracking patients is like a chef who never tastes his own cooking. We need this information to constantly improve our outcomes,” he concluded.
Adi Abulafa: adi.abulafia@gmail.com
Tags: cataract and refractive
Latest Articles
Making Female Leadership More than a Moment
A remarkable global confluence of women in key positions.
ESCRS Talks Technology at AAO
Europe adopts technological advances, US still waiting for lenses and lasers.
Sorting Out Simultaneous Vision IOLs
The ESCRS Eye Journal Club discuss a new landmark paper on IOL classification and the need for harmonisation of terminology for presbyopic IOLs.
Big Advantages to Small-Aperture IOLs
Small-aperture IOLs offer superior image quality with increased range of focus.
Prioritising Self-Care
Benefits of maintaining physical, emotional, and mental health extend beyond the personal sphere.
Valuing Clinical Trial Design
How inclusivity and diversity can enhance scientific accuracy in research.
Knowing Iris Repair: Using Iridodiathermy in Iris Surgery
Prepare for decentred pupils and uneven irides in multiple situations.
Neuroprotectant Treatment for MacTel Type 2
Intravitreal implant releasing ciliary neurotrophic factor found safe and effective in pivotal trials.