Cornea, Corneal Therapeutics
Surgery for Anterior Corneal Disease
Achieving vision improvement and minimising morbidity by tailoring the procedure to the pathology location.

Cheryl Guttman Krader
Published: Tuesday, October 1, 2024
When surgery is indicated for visual rehabilitation of an eye with corneal disease not affecting the endothelium and Descemet’s membrane, think about an anterior procedure instead of penetrating keratoplasty, advises Sadeer B Hannush MD.
“There is no reason to do a full-thickness graft in this situation,” Dr Hannush said. “Even a partial thickness graft may not be necessary.”
The choice of surgical intervention is guided by whether the pathology lies anterior or posterior to Bowman’s layer (BL) and, if posterior to BL, how deep. If there is only visually significant basement membrane disease, superficial keratectomy—which only removes the epithelium and basement membrane—is an effective and simple but underused procedure, according to Dr Hannush.
“Lamellar keratectomy for basement membrane disease results in rapid and significant visual improvement,” he said. “Frequently, patients see clearly before they leave the office.”
Anterior lamellar keratectomy, which removes the anterior stroma, can be done instead of a graft procedure in cases where the corneal pathology is posterior to BL but within the anterior 200 microns of the stroma. It may be performed by freehand dissection, phototherapeutic keratectomy with an excimer laser, or microkeratome- or femtosecond laser-assisted keratectomy. After the tissue is removed, mitomycin-C is applied, followed by copious irrigation.

“Visual improvement also occurs fairly rapidly after these procedures,” Dr Hannush said. “It is not necessary to remove every opacity for the patient to achieve significant improvement in vision.”
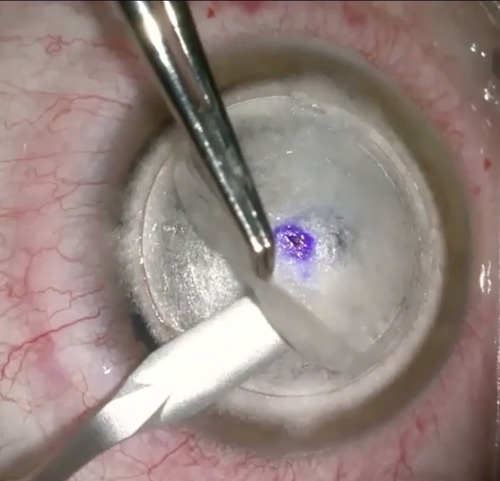
Deep anterior lamellar keratoplasty (DALK) is indicated for treating eyes with corneal ectasia that have failed rigid gas permeable or scleral contact lenses or for those with stromal dystrophies or stromal scars from previous infection or non-penetrating trauma. The dissection in the host cornea removes most or all the corneal stroma down to either the pre-Descemet’s layer (PDL), also known as Dua’s layer (DL), or to Descemet’s membrane (DM) itself. After initial debulking of the host stroma, further dissection may be accomplished manually or by the Big Bubble (BB) technique, viscodissection, or femtosecond laser-assisted air dissection.
Dr Hannush noted when performing the BB technique, surgeons should be aware the desired type 1 BB occurs 90% of the time, forms centrally first, and extends to the periphery with significant emphysema (whitening) of the cornea. Here, the air bubble forms between the posterior stroma and PDL. In about 10% of air injections, a type 2 BB develops, with the bubble forming in the periphery and extending centrally with minimal whitening of the cornea. The bubble forms between the PDL and DM. It is important to recognise the type 2 BB scenario because it presents a fragile situation associated with an increased risk of DM rupture.
“Whereas the PDL has a bursting pressure of about 500–700 mmHg, DM bursts quickly at a pressure of about 30 mmHg.
“Some surgeons might decide not to proceed with removing the posterior stroma if a type 2 BB occurs, but it is not necessary to abort the DALK procedure in this situation,” Dr Hannush said. “The surgeon may either remove the posterior stroma carefully, paying attention not to come in contact with DM (this may be facilitated by softening the eye by removing some aqueous through a paracentesis). Alternatively, the surgeon may continue with layer-by-layer manual dissection, leaving a thin layer of posterior stroma.”
Dr Hannush spoke at 2024 ASCRS Cornea Day in Boston, US.
Sadeer B Hannush MD is an Attending Surgeon at Wills Eye Hospital and Professor of Ophthalmology, Thomas Jefferson University, Philadelphia, US. sbhannush@gmail.com