Cornea, IOL
Need to Know: Spherical Aberration
Part three of this series examines spherical aberration and its influence on higher-order aberrations.
Soosan Jacob
Published: Friday, August 1, 2025
Spherical aberration (SA) is a rotationally symmetrical aberration belonging to the fourth order, together with secondary astigmatism and quadrafoil. SA occurs secondary to the lens refracting peripheral rays differently than the central paraxial rays. In a convex lens, the peripheral rays come to a focus before the rays close to the optical axis. This results in multiple foci, preventing a clear image from forming on the retina.
The distance between the focal points is known as axial or longitudinal spherical aberration (LSA). Transverse spherical aberration (TSA) refers to the perpendicular distance from the optical axis by which peripheral rays miss the ideal focal point. The direction of focus error in TSA is therefore perpendicular to the optical axis, unlike LSA, where the direction of focus error is along the optical axis (see figure).
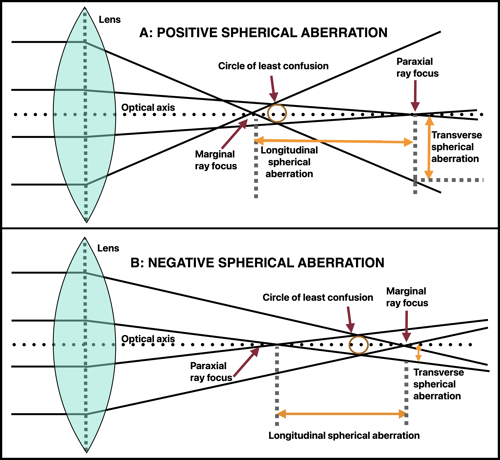
LSA is due to peripheral rays focusing at different depths, causing a depth shift and resulting in defocus blur or axial blurring (depth related). Small amounts of LSA under certain conditions can give an increased depth of focus (DOF). In TSA, on the other hand, peripheral rays spread laterally. Blur is perpendicular in TSA and causes a lateral shift, resulting in light spreading around a point image—thereby reducing image sharpness and causing lateral blurring (spatial spread). Therefore, TSA is an indicator of image blur. It also results in reduced contrast and night vision problems.
In general, LSA is typically referred to as SA in ophthalmological practice. LSA can have a positive or negative value. In positive SA (PSA), peripheral rays focus in front of central rays (more anterior along the optical axis), leading to a myopic shift in refraction (Seidel’s classical optics) and causing halos, glare, and reduced contrast, especially in dim light. Myopic LASIK (oblate cornea) tends to create PSA. In negative SA (NSA) in an emmetropic eye, peripheral rays focus behind central rays (more posterior along the optical axis), which can cause a peripheral hyperopic shift in refraction (Seidel’s classical optics) and affect depth perception. Creating a central myopic refraction (helping near vision) and a negative Seidel SA can provide good distance and near uncorrected visual acuity.
PSA has a ‘sombrero’ configuration in Zernike optics from the hidden second-order defocus, unlike the Gatinel–Malet mode’s flat centre and truer depiction of pure SA (as explained in part two of this series).
SA (LSA) is the ocular aberration with the greatest representation in the human eye. The average total value of Zernike SA for a 6 mm pupil is +0.10 ± 0.10 μm. Slightly positive total residual SA (+0.10 μm) may correlate with better visual acuity. A normal cornea has mild PSA, counteracting the lens’ NSA. The cornea contributes +0.28 ± 0.09 μm while the crystalline lens contributes -0.20 μm for a 6 mm pupil. During accommodation, NSA from the crystalline lens increases by approximately -0.04 μm per dioptre accommodation in a 5 mm pupil. The normal eye shifts from a PSA state at rest to an increasing NSA state with increasing accommodation. Lenticular SA goes from negative to positive as cataracts develop. Hyperopic LASIK (prolate cornea) induces NSA. Keratoconus progression can also increase NSA due to corneal steepening. Some aspheric IOLs are designed to induce NSA to balance corneal PSA, and decentration and tilt can be deleterious in these IOLs.
The human cornea has an aspheric shape, meaning it flattens towards the periphery. This shape reduces PSA and helps maintain better image focus by minimising the difference in focal points for central and peripheral rays. In oblate corneas, peripheral light rays converge in front of central rays, creating PSA. In prolate corneas, peripheral light rays converge posterior to central rays, creating NSA. SA comes into play when pupil size is more than 4 mm (low light).
Clinical relevance of SA
Excessive SA significantly impacts visual quality. It also leads to reduced contrast sensitivity and decreased sharpness.
LSA and night vision disturbances In low light, the pupil allows more peripheral rays to enter. With positive LSA, peripheral rays focus in front of the retina, causing blur, halos, and reduced contrast sensitivity. Because SA is produced by the difference between peripheral and paracentral keratometry, its effect declines with smaller pupils. It contributes almost nothing to total aberrometry for pupil sizes less than or equal to 3 mm.
Keratoconus and irregular corneas Keratoconus produces inferior steepening, resulting in coma. The corneal steepening also increases LSA, which cause multiple focal points, blurred vision, visual distortions, ghosting, and halos (particularly in low-light conditions), ultimately impacting visual quality. LSA changes with disease progression and cone position, making it an important parameter for tracking severity and planning interventions. Many other aberrations also increase in keratoconus.
LSA in refractive surgery (LASIK, PRK, SMILE) Myopic LASIK, especially standard LASIK with large optic zones, induces PSA and positive secondary astigmatism and can cause night vision problems (halos, glare). Wavefront-guided LASIK and aspheric ablation profiles aim to minimise LSA, improving post-surgical visual quality. Hyperopic LASIK induces NSA and negative secondary astigmatism. LASIK can introduce other aberrations as well.
LSA in cataract surgery and IOL selection
The human cornea is aspheric and slightly prolate (Q is less than 0). The natural crystalline lens contributes to NSA, which increases with age. Aspheric IOLs compensate for corneal LSA and improve contrast sensitivity after cataract surgery. Thus, spherical aberration can be corrected with appropriate IOL selection. IOLs can be neutral or induce PSA or NSA. Selecting an IOL that accounts for the patient’s corneal LSA is crucial for achieving optimal vision. However, these may not be a significant advantage with smaller pupil sizes.
IOLs inducing PSA Traditional spherical IOLs increase PSA. They are used in hyperprolate corneas (post-hyperopic LASIK) with NSA. Examples are the MA60AT (Alcon), CT Spheris 204 (Carl Zeiss), and Sensar (Johnson & Johnson) lenses.
IOLs that do not modify SA IOLs with prolate anterior and posterior surfaces that do not modify SA include Akreos, SofPort LI61AO (both Bausch + Lomb), and CT Asphina 409M (Carl Zeiss). These IOLs are less sensitive to tilt, decentration, and pupil eccentricity than aspheric IOLs and have better image quality than spherical IOLs. Zero SA IOLs may also have the advantage of residual SA, improving depth of field.
IOLs inducing NSA IOLs inducing NSA include aspheric IOLs with a prolate anterior surface (Tecnis, Johnson & Johnson), a prolate posterior surface (AcrySof IQ, Alcon), and both prolate surfaces (FineVision, PhysIOL [BVI] and CT Asphina 509M, Carl Zeiss). Depending on the amount of NSA, they provide better contrast sensitivity when correcting corneal PSA but less depth of focus than spherical lenses. They compensate positive aberrations of the average cornea almost completely (Tecnis with -0.27 microns NSA) or partially (AcrySof IQ Aspheric with -0.20 microns NSA). However, it is important to keep in mind SA interacts with residual sphere. Performance also depends on pupil size which needs to be more than 3 mm to see effect. IOL decentration and large angle alpha can induce other aberrations, such as coma, potentially compromising vision. Myopic LASIK patients benefit from NSA IOLs, which may also be better in patients with larger mesopic pupils and those with night-time driving needs.
Bi-sign IOLs These IOLs combine the advantages of neutral and correcting aspherical IOLs, like CT LUCIA (Carl Zeiss), for example. Aspherical profile tolerates greater lens offset. This is good for most patients and ideal when angle alpha is greater than 0.5 mm or in patients at risk of decentred IOL.
Monofocal-plus IOLs Monofocal-plus IOLs mostly function as monofocal IOLs but with slightly increased DOF (between 0.25 D and 0.50 D), which is just enough to provide small improvement at intermediate distances. Increasing SA does not produce a noticeable drop in acuity but does slightly degrade contrast sensitivity. Examples include the Tecnis Eyhance (Johnson & Johnson), which combines NSA with increased central curvature; Isopure (BVI PhysIOL), which uses NSA customised to dioptric power; and RayOne (Rayner), which uses PSA.
Correcting/modifying SA Wavefront-guided LASIK, aspheric IOLs, and customised contact lenses can all modify SA. Controlled induction of HOA in refractive and cataract surgery can enhance DOF. SA can also compensate for loss of accommodation associated with presbyopia. NSA is used in PresbyLASIK and EDOF IOLs. However, all of these work better with a slight myopic central refraction. Custom contact lenses (scleral, hybrid) to reduce LSA and aspheric corneal cross-linking (CXL) protocols to stabilise LSA have been used in keratoconus.
Gatinel’s LD/ HD decomposition NSA creates a series of focal points with central rays focusing closer and peripheral rays farther down. Though NSA decreases visual quality, it remains stable across different defocus values. Depending on the maximum tolerable blur spot, the DOF can thus increase. However, the Zernike formula for SA also contains hidden defocus. For 0.25 microns of NSA with a 6 mm pupil, the amount of defocus present (about 1 micron) corresponds to at least +0.75 D of positive defocus (myopia). Therefore, the myopic shift caused by negative Zernike SA results in an improvement in intermediate and near visual acuity while the central hyperopic shift caused by positive Zernike SA leads to a degradation in intermediate and near visual acuity. This creates the misleading impression that only negative SA enhances DOF, while, in reality, both PSA and NSA can enhance DOF when used appropriately together with manipulation of paraxial defocus.
This is the third in a multipart tutorial on higher-order aberrations. Previous articles in the series can be found here and here.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India, and can be reached at dr_soosanj@hotmail.com.