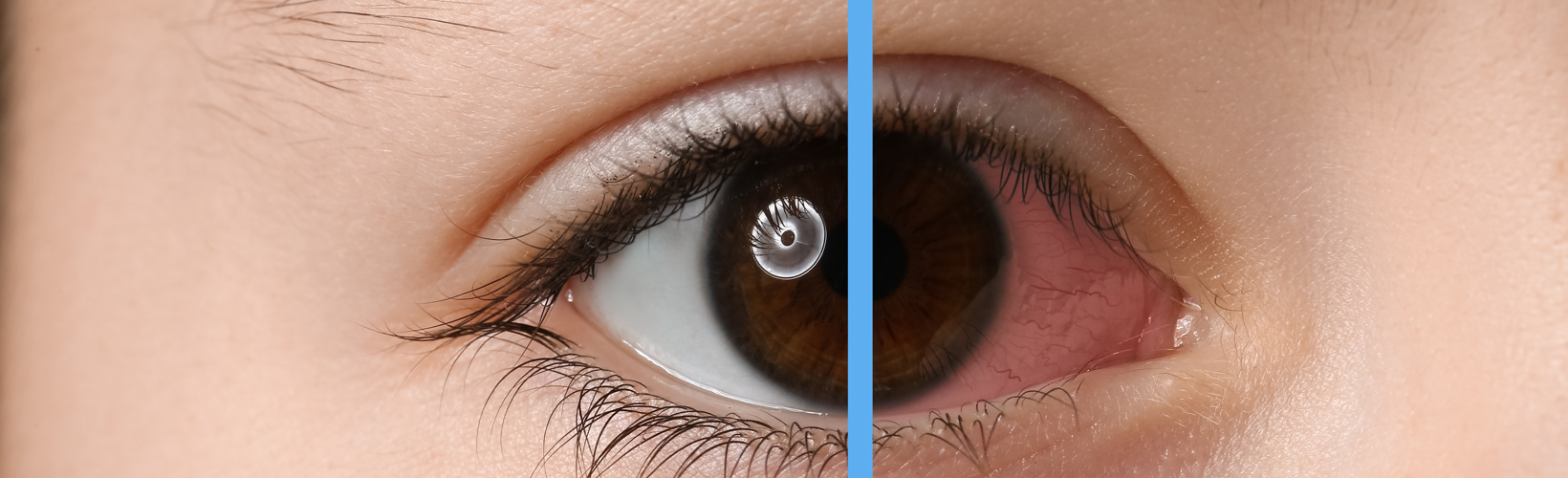
Cataract
Surgeons Split on Post-Surgery Inflammation Control
Leading surgeons weigh whether or how to use a dropless regimen after cataract surgery.
Cheryl Guttman Krader
Published: Tuesday, October 1, 2024
“ In one study, 84% of patients indicated a willingness to pay more for the dropless option. “
There is no disputing relying on topical medications for controlling inflammation after cataract surgery has many drawbacks. However, opinions on using a dropless approach vary.
Ehud I Assia MD said a ‘less drops’ approach works better for him. Although he uses intracameral moxifloxacin for infection prophylaxis, Dr Assia prescribes a 1-month course of topical medications for infection control consisting of two medications, a steroid, and a nonsteroidal anti-inflammatory drug (NSAID), each given three times daily.
Providing the rationale for his approach, Dr Assia noted that unless formulated for sustained release, medications administered intracamerally provide only short-term efficacy. While the limited duration of coverage is adequate for preventing endophthalmitis, he said it is not sufficient to control inflammation.
Short-term efficacy, complication risk, and/or irreversibility decrease the acceptability of other injectable routes for delivering anti-inflammatory drugs—e.g., subconjunctival injection and approaches for posterior chamber placement. The intracanalicular dexamethasone insert offers reversibility, but available data show it is not more effective than topical steroids, Dr Assia said.
“The less drops regimen is effective, reversible, adjustable, and inexpensive,” he concluded.
Support for subconjunctival steroids
Advocating for subconjunctival steroid injection, Neal H Shorstein MD reviewed findings from a recently published study reporting on the effectiveness of subconjunctival triamcinolone acetonide (TA) as a standalone treatment for preventing inflammation after cataract surgery.1 Dr Shorstein noted that in 2008, he and two colleagues at Kaiser Permanente Northern California began an injection-only protocol for their cataract surgery medication regimen using an intracameral antibiotic and subconjunctival TA.
“We preferred the subconjunctival route versus a sub-Tenon’s injection for the steroid because using the subconjunctival approach, we could visualise the needle tip during delivery and the depot postoperatively, allowing us to avoid globe perforation and excise the depot postoperatively if necessary,” he said.
The steroid regimen was modified over time, transitioning from a 2 mg dose using TA 40 mg/mL to 4 mg using TA 10 mg/mL. Dr Shorstein explained the smaller dose of the higher concentration drug was associated with a significant IOP rise in a very small percentage of patients and was found to be less effective than topical prednisolone plus an NSAID. The higher dose using a lower concentration of TA was more effective and caused fewer IOP spikes.
The recent study included data from almost 70,000 eyes operated on between 2018 and 2021. They were assessed for development of macular oedema, rebound iritis, and glaucoma-related events occurring from 15 days to 1 year postoperatively. Eyes receiving subconjunctival TA were divided into subgroups by TA dose and concentration. Researchers used a multivariate analysis to compare the outcomes to a reference group receiving topical anti-inflammatory treatment.
Reviewing the results and weighing the benefits and risks, Dr Shorstein and colleagues concluded TA 4 mg (10 mg/mL) was the favoured regimen for preventing inflammation in routine cases. However, they suggested TA 4 mg (40 mg/mL) may be applicable for patients with pre-existing iritis because it further lowered the risks of macular oedema and iritis. However, close follow-up is important because TA 4 mg (40 mg/mL) was associated with higher odds of IOP elevation.
Also considering the risk for increased IOP, Dr Shorstein noted the need to exercise caution using subconjunctival TA in patients with an optic nerve at risk or elevated risk for a steroid response. With safety in mind, he also recommended using the studied product (Kenalog; because different triamcinolone products have different pharmacokinetics), monitoring IOP until the depot is no longer visible, and injecting the medication inferiorly versus superiorly.
Sustained release steroid
Seth M Pantanelli MD explained why he prefers the intracanalicular dexamethasone insert as his choice for a steroid after cataract surgery.
“The insert has been shown to be safe and effective for controlling pain and inflammation. Insertion is easy and fast—it can be done in less than 15 seconds, and patient perspectives about the insert are overwhelmingly positive,” Dr Pantanelli said.
“Although the insert adds cost for the medical system, the ambulatory surgery centre (ASC), surgeon, and patient, it can actually be cost-neutral or even revenue positive, depending on the comparator.”
Dr Pantanelli reviewed data from premarket approval studies demonstrating the intracanalicular insert was more effective than placebo for controlling inflammation and pain—but he also emphasised results from a retrospective chart review showing it was as effective as topical steroid drops, which is the more relevant comparator.2 Furthermore, results from two studies in which patients underwent surgery with the insert in one eye and topical drops in the other showed the vast majority of participants (≥92%) preferred the insert. In one study, 84% of patients indicated a willingness to pay more for the dropless option.3,4
Regarding cost issues, Dr Pantanelli noted insert use might generate a per case profit of up to US$35 for the ASC or surgeon.
“We have to consider cost in this world of decreasing reimbursement, and we also have to consider cost to patients with topical drops,” he said.
Drs Assia, Shorstein, and Pantanelli spoke at ASCRS 2024 in Boston, US.
Ehud I Assia MD is Professor of Ophthalmology, Tel Aviv University, Tel Aviv, Israel. assia@eintal com
Neal H Shorstein MD is an ophthalmologist, researcher, and associate chief of quality at Kaiser Permanente Medical Center in Walnut Creek, California, US. neal.shorstein@gmail.com
Seth M Pantanelli MD, MS is Professor of Ophthalmology, Penn State College of Medicine, Hershey, Pennsylvania, US. spantanelli@pennstatehealth.psu.edu
1. Shorstein NH, McCabe SE, Alavi M, Kwan ML, Chandra NS. “Triamcinolone Acetonide Subconjunctival Injection as Stand-alone Inflammation Prophylaxis after Phacoemulsification Cataract Surgery,” Ophthalmology. 2024 Apr 4: S0161-6420(24)00206-9. Epub ahead of print.
2. Lu AQ, Rizk M, O’Rourke T, et al. “Safety and efficacy of topical vs intracanalicular corticosteroids for the prevention of postoperative inflammation after cataract surgery,” J Cataract Refract Surg. 2022; 48(11): 1242–1247.
3. Donnenfeld ED, Hovanesian JA, Malik AG, Wong A. “A Randomized, Prospective, Observer-Masked Study Comparing Dropless Treatment Regimen Using Intracanalicular Dexamethasone Insert, Intracameral Ketorolac, and Intracameral Moxifloxacin versus Conventional Topical Therapy to Control Postoperative Pain and Inflammation in Cataract Surgery,” Clin Ophthalmol. 2023; 17: 2349–2356.
4. Gira JP, Sampson R, Silverstein SM, et al. “Evaluating the patient experience after implantation of a 0.4 mg sustained release dexamethasone intracanalicular insert (Dextenza™): results of a qualitative survey,” Patient Prefer Adherence. 2017; 11: 487–494.