Phacoemulsification in vitrectomised eyes

Soosan Jacob
Published: Thursday, April 2, 2020
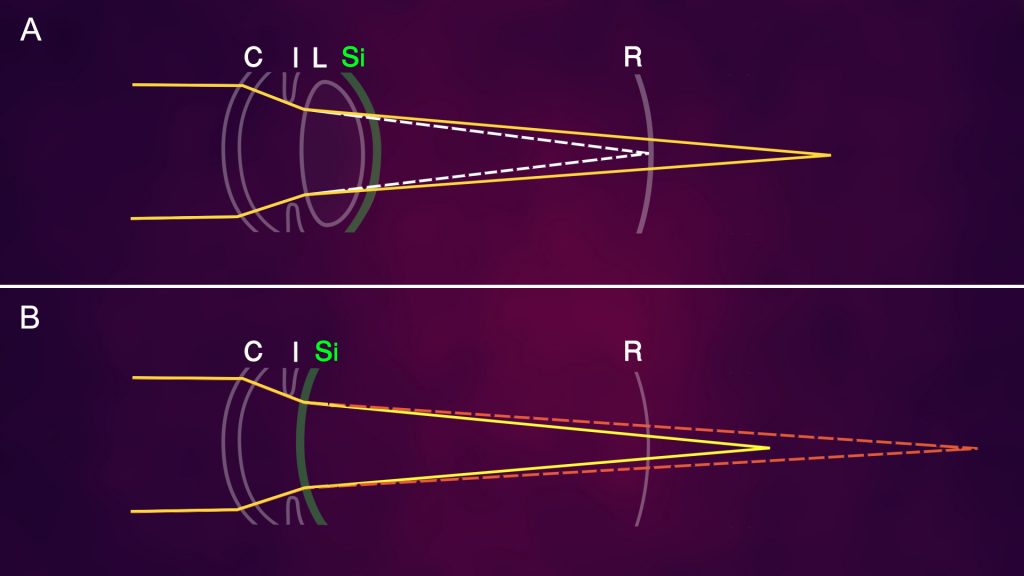 Fig: Light refraction in a silicone oil-filled eye: A: In phakic and pseudophakic eyes, silicone oil forms a concave meniscus (green arc) with posterior lens/IOL surface, causing light rays to diverge from their normal path (dotted white line) to focus behind the retina (yellow); B: In aphakic eyes, silicone oil forms a convex meniscus (green arc), causing light rays to converge from their normal aphakic path (dotted orange line) to focus slightly earlier (yellow), though still behind the retina. In both scenarios in a normal dimensioned eye, a hyperopic refractive error is generally seen. Abbreviations: C- Cornea; I- Iris, L- Lens; Si- Silicone oil; R- Retina
Advances in safety and efficacy have increased the number of vitrectomies being performed. Consequently, associated complications have also increased, one being cataract formation.
With a wide range of incidence (12-80%) reported, we are increasingly called upon to perform cataract surgery in vitrectomised eyes. However, these eyes can be challenging because of conjunctival scarring, low scleral rigidity, greater collapsibility, deeper anterior chamber (AC), lens-iris diaphragm retropulsion syndrome (LIDRS), increased mobility of posterior capsule secondary to lack of vitreous support, zonulopathy, fluid misdirection syndrome, poorly dilating pupils, lax and fragile capsular bag etc.
In addition, they may have complications – either iatrogenic or secondary to the retinal pathology – such as endothelial loss, lens touch with compromised posterior capsule, glaucoma, diabetic/other retinopathy, optic neuropathy, cystoid macular oedema, risk for retinal redetachment etc.
These cases need careful management. Proper counselling, review of previous medical and surgical records as well as a comprehensive eye evaluation for emulsified oil droplets in AC, zonulopathy, pupillary dilatation, specular count, anterior/posterior capsular plaques or evidence of lens touch under coaxial illumination with dilated pupil, thorough retinal examination, assessment of visual potential etc. is advisable. A B-scan is done if the cataract is dense.
TECHNIQUE
Though experienced surgeons can use topical and intracameral lidocaine, peri-bulbar block may be preferred as surgery is expected to be more difficult. Well-constructed incisions are important to avoid fluid leakage and fluctuations of AC depth. Extensive posterior segment pathology can cause a poor red reflex.
In eyes with anterior capsular fibrotic plaques, rhexis can be initiated with 26-gauge needle and/or micro-scissors. Extensive/ peripheral plaques can be cut through with micro-scissors or vitrector while small, central plaques can be included within the rhexis.
Hydrodissection should be done carefully as unidentified lens touch/broken posterior capsule from previous intravitreal injection/vitrectomy can result in nucleus drop. Cataract developing soon after the primary procedure should make one suspect presence of such a break and in such cases hydrodissection should be avoided. These eyes have a higher risk for anterior and posterior capsular tears and zonular dehiscence.
Other problems that are encountered include equatorial and zonular stretch and LIDRS on instilling viscoelastic or initiating irrigation. Increased AC volume causes reverse pupillary block by causing 360-degree irido-capsular contact. Young age and high myopic eyes compound this effect. Sudden backward movement and deepening of the AC causes discomfort to the patient if surgery is under topical anaesthesia. An excessively deep AC necessitates holding instruments more vertically and increases the range of focus required.
Reverse pupillary block can be neutralised by lifting the iris edge off the anterior capsule and allowing fluid to equilibrate between anterior and posterior chambers, thus bringing the iris, zonules and lens back to a more normal position. This manoeuvre generally brings the pupil back to its original size, though miosis may sometimes occur because of prostaglandin release. The reverse pupillary block repeats on initiating infusion each time and should be tackled in a similar manner. It can be prevented by placing a rod between iris and anterior capsule each time before initiating infusion. Despite breaking the reverse pupillary block, instruments may still need to be placed more vertical than usual, leading to greater difficulty in nucleus removal and cortex aspiration techniques.
Repeated shallowing of the AC can increase the risk of retinal re-detachment. New phaco machines with active fluidics help. In addition, the AC should be filled by injecting viscoelastic with the left hand before withdrawing the phaco or I/A probe. For soft nuclei, prolapse and supra-capsular phacoemulsification is easier than in-the-bag nuclear disassembly.
However, nuclear sclerosis is usually dense and horizontal chopping may exert the least stress on the bag and zonules. A posterior capsular plaque may necessitate capsular polishing, plaque peeling, posterior capsulorhexis or a deferred YAG capsulotomy.
IOL implantation should be done after filling the bag well with viscoelastic to prevent haptic snag on a lax capsule. Proper wound closure should be ascertained at the end of surgery and if required, suture should be applied.
POST-OP COMPLICATIONS
These include wound leak, increased inflammation, cystoid macular oedema, pseudophakic retinal detachment, silicone oil migration to the AC, IOL calculation errors, late in-the-bag IOL subluxation etc. Postoperative retinal examination is important. Macular or other retinal pathology may limit postoperative visual acuity attained.
CHOICE OF IOL
Silicone IOLs should be avoided in eyes that have undergone previous vitrectomy or that may require vitrectomy in the future as silicone oil may stick to its surface.
Both hydrophobic and hydrophilic IOLs are suitable, with hydrophilic being least prone to adhesion of silicone oil. Hydrophobic IOLs are preferred with compromised corneal endothelium as hydrophilic IOLs can opacify secondary to air tamponade used in endothelial keratoplasty. PMMA IOLs are also acceptable.
Three-piece foldable IOLs are easily amenable to closed chamber translocation to glued IOL if progressive zonulopathy causes IOL subluxation/ dislocation. In-the-bag single-piece acrylic IOLs may also be refixated using sutured segments or the sutureless glued capsular hook technique described by the author. Plate-haptic IOLs should be avoided. Large optic IOLs that allow unhindered view of the retina is preferred.
hacoemulsification may be planned together with silicone oil removal, often about six months after the vitrectomy. Ultrasound biometry gives errors in axial length measurement and optical biometry should be done after selecting “silicone oil” mode for IOL power calculation. If silicone oil is not removed, the shape of the posterior surface of the IOL is important as the meniscus formed by silicone oil can result in refractive surprises.
An IOL with plano posterior surface is preferable, but not easily available. With a biconvex IOL, silicone oil acts as a negative lens and alters IOL power by 3-to-5 dioptres. The hyperopic error gets corrected, however, once the silicone oil is removed. Interim management is with glasses, contact lens or even a piggyback IOL.
To conclude, though these cataracts are more challenging, they can be handled. Combined cataract with vitrectomy can be considered in the first stage itself, especially in patients with risk factors for developing cataract, such as older age, pre-existing nuclear sclerosis, diabetic retinopathy and if silicone oil or intraocular gas are being considered.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India and can be reached at dr_soosanj@hotmail.com
Fig: Light refraction in a silicone oil-filled eye: A: In phakic and pseudophakic eyes, silicone oil forms a concave meniscus (green arc) with posterior lens/IOL surface, causing light rays to diverge from their normal path (dotted white line) to focus behind the retina (yellow); B: In aphakic eyes, silicone oil forms a convex meniscus (green arc), causing light rays to converge from their normal aphakic path (dotted orange line) to focus slightly earlier (yellow), though still behind the retina. In both scenarios in a normal dimensioned eye, a hyperopic refractive error is generally seen. Abbreviations: C- Cornea; I- Iris, L- Lens; Si- Silicone oil; R- Retina
Advances in safety and efficacy have increased the number of vitrectomies being performed. Consequently, associated complications have also increased, one being cataract formation.
With a wide range of incidence (12-80%) reported, we are increasingly called upon to perform cataract surgery in vitrectomised eyes. However, these eyes can be challenging because of conjunctival scarring, low scleral rigidity, greater collapsibility, deeper anterior chamber (AC), lens-iris diaphragm retropulsion syndrome (LIDRS), increased mobility of posterior capsule secondary to lack of vitreous support, zonulopathy, fluid misdirection syndrome, poorly dilating pupils, lax and fragile capsular bag etc.
In addition, they may have complications – either iatrogenic or secondary to the retinal pathology – such as endothelial loss, lens touch with compromised posterior capsule, glaucoma, diabetic/other retinopathy, optic neuropathy, cystoid macular oedema, risk for retinal redetachment etc.
These cases need careful management. Proper counselling, review of previous medical and surgical records as well as a comprehensive eye evaluation for emulsified oil droplets in AC, zonulopathy, pupillary dilatation, specular count, anterior/posterior capsular plaques or evidence of lens touch under coaxial illumination with dilated pupil, thorough retinal examination, assessment of visual potential etc. is advisable. A B-scan is done if the cataract is dense.
TECHNIQUE
Though experienced surgeons can use topical and intracameral lidocaine, peri-bulbar block may be preferred as surgery is expected to be more difficult. Well-constructed incisions are important to avoid fluid leakage and fluctuations of AC depth. Extensive posterior segment pathology can cause a poor red reflex.
In eyes with anterior capsular fibrotic plaques, rhexis can be initiated with 26-gauge needle and/or micro-scissors. Extensive/ peripheral plaques can be cut through with micro-scissors or vitrector while small, central plaques can be included within the rhexis.
Hydrodissection should be done carefully as unidentified lens touch/broken posterior capsule from previous intravitreal injection/vitrectomy can result in nucleus drop. Cataract developing soon after the primary procedure should make one suspect presence of such a break and in such cases hydrodissection should be avoided. These eyes have a higher risk for anterior and posterior capsular tears and zonular dehiscence.
Other problems that are encountered include equatorial and zonular stretch and LIDRS on instilling viscoelastic or initiating irrigation. Increased AC volume causes reverse pupillary block by causing 360-degree irido-capsular contact. Young age and high myopic eyes compound this effect. Sudden backward movement and deepening of the AC causes discomfort to the patient if surgery is under topical anaesthesia. An excessively deep AC necessitates holding instruments more vertically and increases the range of focus required.
Reverse pupillary block can be neutralised by lifting the iris edge off the anterior capsule and allowing fluid to equilibrate between anterior and posterior chambers, thus bringing the iris, zonules and lens back to a more normal position. This manoeuvre generally brings the pupil back to its original size, though miosis may sometimes occur because of prostaglandin release. The reverse pupillary block repeats on initiating infusion each time and should be tackled in a similar manner. It can be prevented by placing a rod between iris and anterior capsule each time before initiating infusion. Despite breaking the reverse pupillary block, instruments may still need to be placed more vertical than usual, leading to greater difficulty in nucleus removal and cortex aspiration techniques.
Repeated shallowing of the AC can increase the risk of retinal re-detachment. New phaco machines with active fluidics help. In addition, the AC should be filled by injecting viscoelastic with the left hand before withdrawing the phaco or I/A probe. For soft nuclei, prolapse and supra-capsular phacoemulsification is easier than in-the-bag nuclear disassembly.
However, nuclear sclerosis is usually dense and horizontal chopping may exert the least stress on the bag and zonules. A posterior capsular plaque may necessitate capsular polishing, plaque peeling, posterior capsulorhexis or a deferred YAG capsulotomy.
IOL implantation should be done after filling the bag well with viscoelastic to prevent haptic snag on a lax capsule. Proper wound closure should be ascertained at the end of surgery and if required, suture should be applied.
POST-OP COMPLICATIONS
These include wound leak, increased inflammation, cystoid macular oedema, pseudophakic retinal detachment, silicone oil migration to the AC, IOL calculation errors, late in-the-bag IOL subluxation etc. Postoperative retinal examination is important. Macular or other retinal pathology may limit postoperative visual acuity attained.
CHOICE OF IOL
Silicone IOLs should be avoided in eyes that have undergone previous vitrectomy or that may require vitrectomy in the future as silicone oil may stick to its surface.
Both hydrophobic and hydrophilic IOLs are suitable, with hydrophilic being least prone to adhesion of silicone oil. Hydrophobic IOLs are preferred with compromised corneal endothelium as hydrophilic IOLs can opacify secondary to air tamponade used in endothelial keratoplasty. PMMA IOLs are also acceptable.
Three-piece foldable IOLs are easily amenable to closed chamber translocation to glued IOL if progressive zonulopathy causes IOL subluxation/ dislocation. In-the-bag single-piece acrylic IOLs may also be refixated using sutured segments or the sutureless glued capsular hook technique described by the author. Plate-haptic IOLs should be avoided. Large optic IOLs that allow unhindered view of the retina is preferred.
hacoemulsification may be planned together with silicone oil removal, often about six months after the vitrectomy. Ultrasound biometry gives errors in axial length measurement and optical biometry should be done after selecting “silicone oil” mode for IOL power calculation. If silicone oil is not removed, the shape of the posterior surface of the IOL is important as the meniscus formed by silicone oil can result in refractive surprises.
An IOL with plano posterior surface is preferable, but not easily available. With a biconvex IOL, silicone oil acts as a negative lens and alters IOL power by 3-to-5 dioptres. The hyperopic error gets corrected, however, once the silicone oil is removed. Interim management is with glasses, contact lens or even a piggyback IOL.
To conclude, though these cataracts are more challenging, they can be handled. Combined cataract with vitrectomy can be considered in the first stage itself, especially in patients with risk factors for developing cataract, such as older age, pre-existing nuclear sclerosis, diabetic retinopathy and if silicone oil or intraocular gas are being considered.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India and can be reached at dr_soosanj@hotmail.com