Lockdown Loco
Operating on patients during the COVID-19 pandemic is opening up new challenges for ophthalmologists

Clare Quigley
Published: Thursday, December 3, 2020
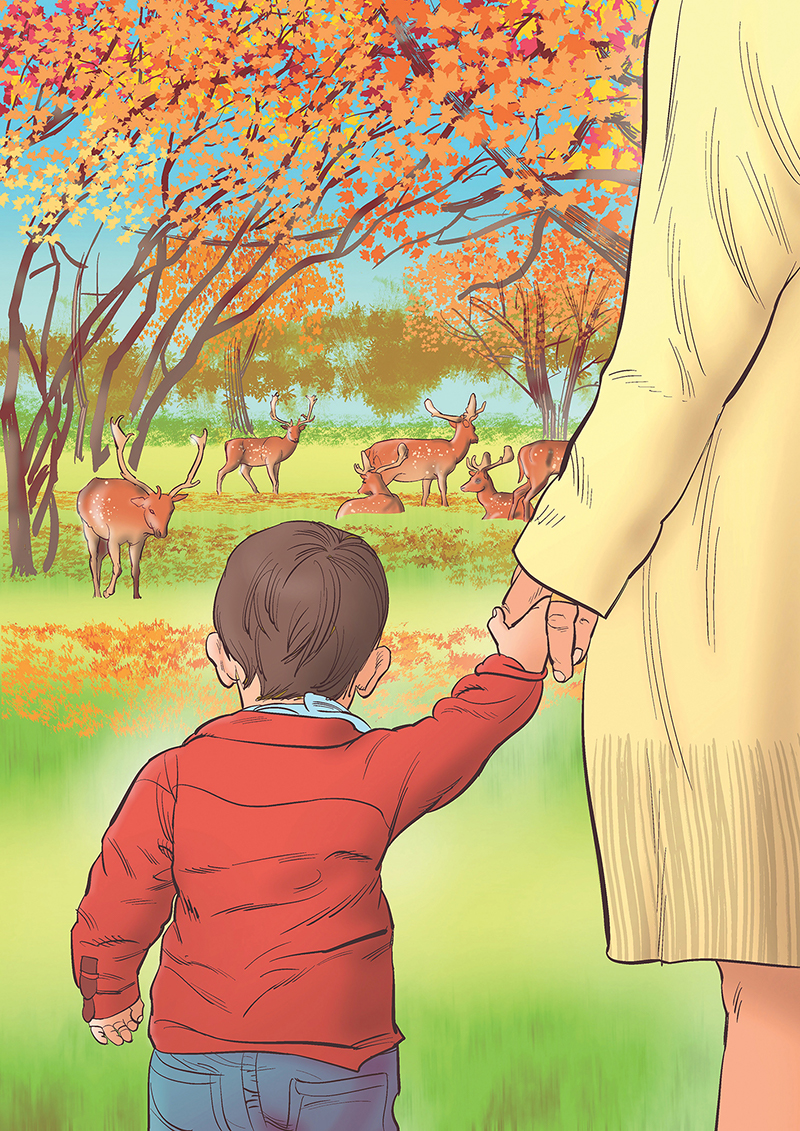 We brought Michael there for a visit – at 11 months he is a bit young for the zoo, maybe it was more ourselves we were taking for the outing – but he was captivated by one of the animals, a red panda. Red pandas are small, furry creatures native to the Himalayas, like a cross between a raccoon and a fox. One padded right by Michael as he followed it wide-eyed, watching through the glass until it was out of sight. Trips to the Phoenix park, and the other parks close by, feel precious at the moment. The trees are brilliantly lit uup in shades of red, orange and yellow for another short while.
Clinical activities in the Royal Victoria Eye and Ear Hospital – or the Eye and Ear as we call it – are still up and running, as a second wave of COVID is breaking. Patients attend for cataract surgery, and I’ve been getting back into the rhythm of operating. In one week I did my fastest, and one of my slowest cataract surgeries. The former case was a myopic woman in her fifties with posterior subcapsular cataract, who was quite nervous. The anaesthetist gave a good subtenons block and some sedation. I saw that the cataract looked soft, and that her anterior chamber was nice and deep; I could take my usual soft lens approach.
After making a generous rhexis I was able to pop up the lens on hydrodissection, so it sat vertically half in, half out of the bag. From there I aspirated in the iris plane, spinning the lens with a drysdale instead of my usual chopper, minimal phaco required. In and out in under ten minutes.
The latter case was tricky. She was a 97-year-old lady, who was profoundly deaf, but seemed calm and able for surgery under local anaesthetic. I gave her written instructions, and she seemed to understand what was required. On the table though, after a promisingly quiet start, she did not stop moving her head and talking. Complicating matters, she had a tiny pupil that did not respond to intracameral phenylephrine, and a dense cataract. A Malyugin ring brought up her pupil to give adequate access, and I enlisted the scrub nurse to clamp his hands on her temples – I got through it okay in the end, after more than half an hour, but we both said we wouldn’t like to do it again.
Work is more than cataracts – until early next year I will be on the glaucoma team, training under Consultants Jeremy O’Connor and Aoife Doyle. The days begin with a ward round, followed by a mix of clinic and theatre sessions. I see complex patients in their clinics; my decision process about which patients need a trabeculectomy, and who could get by with laser or drops, is becoming more refined. Getting to know the visual field progression analysis software has helped, but more importantly the relatively quiet clinics mean I can have a good discussion on cases with the consultants; compared to normal times, the clinic numbers are halved, to comply with the social distancing measures. We don’t like to imagine how half the patients who used to attend regularly are getting on without a review... as a mitigating measure they have opened a new drive-through IOP clinic for suitable patients. Patients get a quick iCare pressure check, without even exiting their car. It’s not a clinic visit with a visual field, but it’s something.
Infection rates may worsen, and elective surgeries and clinics may grind to a halt again. I try not to think about that. Or the health budget, and how much it will likely contract over the next few years – when I will be due to finish training – new consultant ophthalmologist jobs are already sporadic at best... Thinking about that too much, it would be easy to go lockdown loco.
Clare Quigley is a resident at the Royal Victoria Eye and Ear Hospital, Dublin, Ireland
Illustration by Eoin Coveney
We brought Michael there for a visit – at 11 months he is a bit young for the zoo, maybe it was more ourselves we were taking for the outing – but he was captivated by one of the animals, a red panda. Red pandas are small, furry creatures native to the Himalayas, like a cross between a raccoon and a fox. One padded right by Michael as he followed it wide-eyed, watching through the glass until it was out of sight. Trips to the Phoenix park, and the other parks close by, feel precious at the moment. The trees are brilliantly lit uup in shades of red, orange and yellow for another short while.
Clinical activities in the Royal Victoria Eye and Ear Hospital – or the Eye and Ear as we call it – are still up and running, as a second wave of COVID is breaking. Patients attend for cataract surgery, and I’ve been getting back into the rhythm of operating. In one week I did my fastest, and one of my slowest cataract surgeries. The former case was a myopic woman in her fifties with posterior subcapsular cataract, who was quite nervous. The anaesthetist gave a good subtenons block and some sedation. I saw that the cataract looked soft, and that her anterior chamber was nice and deep; I could take my usual soft lens approach.
After making a generous rhexis I was able to pop up the lens on hydrodissection, so it sat vertically half in, half out of the bag. From there I aspirated in the iris plane, spinning the lens with a drysdale instead of my usual chopper, minimal phaco required. In and out in under ten minutes.
The latter case was tricky. She was a 97-year-old lady, who was profoundly deaf, but seemed calm and able for surgery under local anaesthetic. I gave her written instructions, and she seemed to understand what was required. On the table though, after a promisingly quiet start, she did not stop moving her head and talking. Complicating matters, she had a tiny pupil that did not respond to intracameral phenylephrine, and a dense cataract. A Malyugin ring brought up her pupil to give adequate access, and I enlisted the scrub nurse to clamp his hands on her temples – I got through it okay in the end, after more than half an hour, but we both said we wouldn’t like to do it again.
Work is more than cataracts – until early next year I will be on the glaucoma team, training under Consultants Jeremy O’Connor and Aoife Doyle. The days begin with a ward round, followed by a mix of clinic and theatre sessions. I see complex patients in their clinics; my decision process about which patients need a trabeculectomy, and who could get by with laser or drops, is becoming more refined. Getting to know the visual field progression analysis software has helped, but more importantly the relatively quiet clinics mean I can have a good discussion on cases with the consultants; compared to normal times, the clinic numbers are halved, to comply with the social distancing measures. We don’t like to imagine how half the patients who used to attend regularly are getting on without a review... as a mitigating measure they have opened a new drive-through IOP clinic for suitable patients. Patients get a quick iCare pressure check, without even exiting their car. It’s not a clinic visit with a visual field, but it’s something.
Infection rates may worsen, and elective surgeries and clinics may grind to a halt again. I try not to think about that. Or the health budget, and how much it will likely contract over the next few years – when I will be due to finish training – new consultant ophthalmologist jobs are already sporadic at best... Thinking about that too much, it would be easy to go lockdown loco.
Clare Quigley is a resident at the Royal Victoria Eye and Ear Hospital, Dublin, Ireland
Illustration by Eoin Coveney