Cornea, Corneal Therapeutics
Limits and Complications of Cross-linking
Attention to the ocular surface key to reducing problems.

“ The key message is ocular surface inflammation is [just as] important for complications as predisposing factors. “
Although no treatment is perfect, corneal cross-linking (CXL) has effected a veritable paradigm shift in keratoconus management and treatment over the past 15 years, according to Cosimo Mazzotta MD, PhD.
Speaking at the 2024 EuCornea Congress in Paris, Professor Mazzotta said that while his presentation was geared towards discussing the limitations and complications of CXL, it was important to put these downsides into context.
“The encouraging message is that epithelium-off cross-linking is safe and effective in stabilizing keratoconus progression,” he said. “Today, we have a technique with a high safety profile, and a recent study has shown a dramatic reduction in corneal transplants for keratoconus after the extensive application of cross-linking.”
The long-term data also confirms this positive viewpoint, demonstrating the CXL procedure is effective in treating keratoconic eyes in the progressive stage of the disease and achieving long-term stabilization up to 15 years after treatment without the occurrence of serious complications and side effects, he added.1
Prof Mazzotta explained the scientific literature reported retreatment rates between 8% and 14% up to 15 years after treatment.

And while cross-linking is a repeatable procedure if keratoconus continues to progress, there are serious complications to bear in mind, such as burns, serious infections, and corneal ulcers—which in some scenarios may ultimately result in transplantation.
Geographic, ethnic, and environmental conditions typically influence the rate, type, and severity of complications, Prof Mazzotta noted.
“Our complications in Europe are different from those in India, Africa, and the Middle East because we have different keratoconus stages at presentation, different sunlight overexposure, different hygienic conditions and environments that influence the rate, type, and severity of complications and the compliance of patients to medications and controls,” he said.
Treating thin corneas with keratoconus is no longer an issue thanks to a novel pachymetry-based nomogram (M nomogram), which uses an accelerated pulsed light protocol based on baseline minimum corneal thickness.2
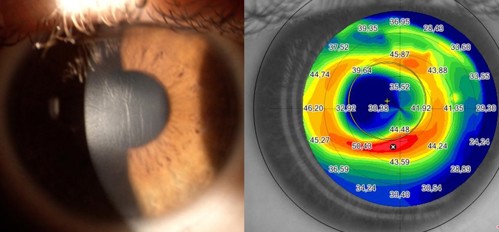
Complications of epithelium-off CXL include infectious keratitis, non-infectious keratitis, haze, stromal melting, epithelial healing defects, dry eye, reduced uncorrected and corrected distance visual acuity, and failures and retreatments.
There are, however, some predisposing factors for CXL complications, Prof Mazzotta said. “The key message is ocular surface inflammation is [just as] important for complications as predisposing factors. Blepharitis, meibomian gland dysfunction, and dry eye para-inflammation are really predisposing factors that must be cared for and addressed before CXL treatment.”
He also urged clinicians to care for the ocular surface in terms of contact lens bandage, hygiene, environment, and compliance.
“We should try to avoid treatment errors in terms of proper patient selection, consistency in surgical techniques, and choosing the right CXL protocol,” he added.
Complications can typically be divided into temporary issues that last anywhere from 3 to 12 months and more persistent complications longer than 12 months.
“We may have corneal oedema; haze or scarring; melting or perforation; infectious keratitis; bacterial, viral, fungal or wound-related complications; or inflammatory conditions, and everything is influenced by genetic, geographical, and environmental factors and ocular surface inflammation,” he said.
The future perspective is for more epithelium-on treatments. Epi-on high fluence protocols with pulsed light (with or without oxygen) and new generation chemically enhanced or boosted riboflavin solutions offer promising results for early progressive keratoconus, avoiding complications.
Prof Mazzotta observed the choice of CXL protocol must be individualized based on patient age, baseline pachymetry, risk factors for progression, comorbidities, and patient compliance.
The ocular surface must also be borne in mind. “This is my key message today: The inflammatory diseases of the ocular surface—such as blepharitis, dry eye-related para-inflammation, and vernal and allergic forms—must be recognized and treated before any CXL treatment. We must prepare the surface and the cornea to receive the cross-linking just to prevent complications. Epi-on is the way out,” he concluded.
Prof Mazzotta presented at EuCornea 2024 in Paris.
Cosimo Mazzotta MD, PhD, FWCRS is Head of the Siena Crosslinking Center, Siena, Italy; Anterior Segment Surgeon, Departmental Ophthalmology Unit of the Alta Val d’Elsa Hospital, Campostaggia, Siena, Italy; Professor of Corneal Pathology, Postgraduate Ophthalmology Specialty School at the University of Siena, Italy; and International Keratoconus Society (IKS) co-founder. cgmazzotta@libero.it
1. Raiskup F, et al. “Corneal Crosslinking with Riboflavin and UVA Light in Progressive Keratoconus: Fifteen-Year Results,” American J of Ophthal, 2023 June; 250: 95–102. doi: 10.1016/j. ajo.2023.01.022
2. Mazzotta C, et al. “Ray-Tracing Transepithelial Excimer Laser Central Corneal Remodeling plus Pachymetry-Guided Accelerated Corneal Crosslinking for Keratoconus,” Cornea, 2024 Mar 1; 43(3): 285–294. doi: 10.1097/ICO.0000000000003380