Cornea, Corneal Therapeutics
Knowing Iris Repair: Modified Trifold Technique
Part eight of our series covers the modified trifold technique for large iris defects.

Soosan Jacob
Published: Thursday, May 1, 2025
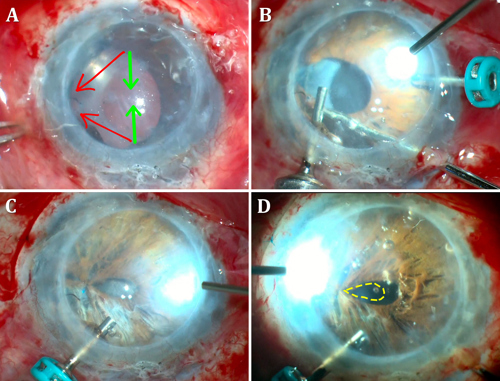
Large iris defects are often seen post injury or secondary to iatrogenic iris trauma. These are challenging to close due to the shortage of iris tissue. The shortage results in excessive opposing vector forces when trying to bring opposite pedicles of the iris in a conventional pupilloplasty technique (Fig A, green arrows), leading either to an inability to suture the pedicles together or sometimes an iris root tear/iridodialysis secondary to the excessive pressure or pull on the iris root. In such cases, two pupilloplasty techniques can be used sequentially to close large iris defects with less tractional force. This article discusses the trifold technique, which is a combination of trocar-assisted iris repair and single-pass, four-throw pupilloplasty (SFT). Dr Agarwal and I described the trifold technique for repairing non-apposable large iris defects, and I modified it further to circularize and centralize the pupil.
In the trifold technique, two initial iris repair sutures are used to appose the unapposed iris ends to the sclera (Fig A [red arrows], B). A subsequent SFT seals the now-smaller iris defect (Fig C). In the modified trifold technique, the initial repair is followed by centralizing and circularizing the pupil using a combination of microscissors, vitrector-assisted pupillectomy, and iridodiathermy (Fig D). This combination of an iridodialysis-style repair of the iris pedicles to the sclera, SFT, and pupil circularization is less manipulative and carries fewer complication risks for both the iris diaphragm and the pupil.
Let us understand this technique in greater detail:
Trifold technique
As previously mentioned, ocular trauma, iatrogenic iris damage, and (rarely) iris colobomas can lead to large, non-apposable iris defects. In such clinical scenarios, closing the iris using a series of SFT/other pupilloplasty knots starting from the pupil margin and proceeding towards the iris base is challenging due to abnormal directional vectors. The trifold technique involves three steps: the initial two steps are mainly to reduce the distance between the two disinserted iris pedicles by attaching the ends to the sclera, and the third step is pupil reformation by SFT pupilloplasty.
Under peribulbar anaesthesia, a narrow, partial thickness lamellar scleral incision is initially made in the clock hours of the expected iris reattachment. A Hoffman pocket may also avoid conjunctival dissection. A 25-gauge (G) trocar is introduced from the limbus in the direction diagonally opposite to the required zone of iris insertion. Once in position, a double-armed 9-0 polypropylene suture needle is guided through the trocar to engage the peripheral end of the disinserted iris. A 30-G needle is then passed through the scleral incision into the anterior chamber (AC) and used to railroad the prolene suture out. The other arm of the suture is passed in the same method through the trocar into the adjacent iris stroma. With both sutures thus externalized, the suture knot is tied down, apposing the iris to the opposite sclera.
The second step repeats the same technique with the iris pedicle on the other side. Both iris pedicles are sutured as close as possible to each other onto the sclera while taking care to avoid excess traction on the opposite attached iris root, reducing the gap in the iris defect. A Snyder hang-back technique may also be similarly used in case of greater tissue shortage. Here, the detached peripheral iris is suspended by a suture from the scleral wall, helping to reduce corectopia while also avoiding inadvertent coverage of the trabecular meshwork by the peripheral iris.
In the third step, the residual vertical defect is closed with SFT pupilloplasty. A single-armed 9-0 or 10-0 polypropylene suture is passed through the proximal iris and docked through a 30-G needle that travelled through the distal iris via paracentesis, railroading the suture out. A Sinskey or Kuglen hook is introduced inside the AC through the paracentesis, and the formed suture loop is then pulled out through the paracentesis. The other end of the suture is cut and passed four times through the loop. The two suture ends on either side of the limbus are pulled apart to draw the loop back into the AC and to tighten the knot, bringing the two ends of the iris into apposition. The suture ends are then cut close to the knot using microscissors. Placing a series of such knots can close the vertical defect.
Care should be taken during every manoeuvre to avoid iris root traction and disinsertion. Any hyphaema that occurs can be controlled by washing the blood out and temporarily increasing the AC pressure.
Role of trocar
The trocar facilitates passage of the long straight or curved needle of the polypropylene suture smoothly through the paracentesis without engaging corneal stroma at the incision. Accidental engagement of incisional stroma tethers the loop at the incision and prevents it from being pulled in. Therefore, the knot cannot be tied, and the entire needle pass needs redoing. The trocar allows the needles to enter the AC smoothly without engaging the incisional corneal stroma. The use of valved trocars generally does not create a problem. However, the valve may be removed prior to use, if needed.
Modified trifold technique
The trifold technique may result in the pupil displacing towards the scleral attachment. This modification further enhances the functional and cosmetic outcome by circularizing and centralizing the pupil—performed by assessing the pupil position, and if displaced, a microscissor creates a vertical cut on the opposite intact pupillary margin. The vitrector is then used at a low cut rate and a 300 mm Hg vacuum to carefully cut the pupil into a round, centralized shape. The pupil can be further centralized and made more circular with iridodiathermy. An additional SFT may be added just ahead of the previous ones if required.
Good functional and cosmetic outcomes can be obtained using the modified trifold technique for large, non-apposable iris defects. These eyes often have other complex anterior segment defects, and this technique can be used with others—for example, after glued intraocular lens in eyes with deficient posterior capsule or before endothelial keratoplasty, where stable air tamponade to the graft is imperative intra- and postoperatively to decrease the risk of air migration and graft detachment.
Iris defects
Iris defects can result in glare, photosensitivity, and diplopia. They may also be cosmetically concerning, especially in patients with light-coloured irides, and often need to be sutured or repaired. However, not all iris defects are apposable, and the risk of associated dialysis from the iris root is a barrier at times—especially in large defects of more than 90 degrees where the force and changed vectors caused by pulling the iris to the opposite direction while suturing can lead to further iris tear and damage. Managing this with a single surgical technique may not be possible. Therefore, to overcome this obstacle of intraoperative suturing, multiple procedures are required to change vector forces and manage the magnitude of defect.
The modified trifold technique for repairing large iris defects seems to involve less manipulation and is associated with fewer complications than other iris suturing techniques. It also does not need expensive iris prosthetic devices and can be done anywhere. In my experience, the modified trifold method of combined trocar-assisted iris repair with SFT and corectopia correction in large iris defects has shown satisfactory outcomes in large non-apposable iris defects. The modified trifold technique is a valuable method for iris diaphragm and pupil reformation. Alternative non-suturing methods for managing iris or pupil defects include coloured contact lenses, corneal tattooing, iris prosthesis, aniridia rings, aniridia IOLs, and iris prosthetic devices—which may have their own benefits and limitations.
This is the eighth article in a series on iris repair. Please see past issues of EuroTimes for related columns.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India, and can be reached at dr_soosanj@hotmail.com.