Endophthalmitis rates increasing
Modern vitrectomy techniques improving results in acute endophthalmitis

Dermot McGrath
Published: Friday, November 1, 2019
 Andrew Chang MD, PhD, FRANZCO
Andrew Chang MD, PhD, FRANZCO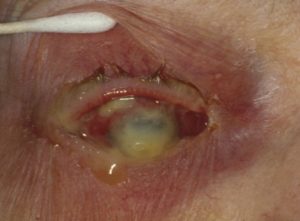 Severe endophthalmitis
Severe endophthalmitisModern vitrectomy techniques improving results in acute endophthalmitis

Published: Friday, November 1, 2019
 Andrew Chang MD, PhD, FRANZCO
Andrew Chang MD, PhD, FRANZCO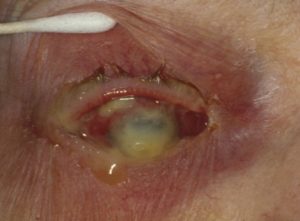 Severe endophthalmitis
Severe endophthalmitis