Cataract, Refractive
DMEK + Light Adjustable Lens
LAL may improve visual outcomes in combined DMEK-cataract surgery. Howard Larkin reports from the 2022 ASCRS Annual Meeting.

Howard Larkin
Published: Tuesday, July 19, 2022
Predicting refractive outcomes in combined Descemet membrane endothelial keratoplasty (DMEK) and cataract surgery is difficult due to the uncertainty of the refractive impact of DMEK. Implanting a Light Adjustable Lens (RxSight, LAL) could help, reducing the need for two separate procedures, according to David A Price MD.
“Staging phaco after DMEK can improve [refractive] precision. We were looking for an alternative to that,” said Dr Price, who co-authored the presentation with Francis W Price Jr. That alternative may be the LAL, which allows tuning lens power days or weeks after implant.
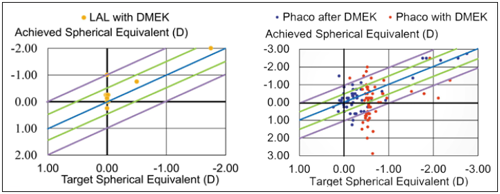
Previous research shows performing phaco after DMEK results in 94% of eyes within 1.0 D of target refraction - compared with just half for conventional combined DMEK-phaco.i
To see how the LAL fares, Dr Price conducted a retrospective single-centre study of 14 eyes in 9 patients receiving the LAL with DMEK. All had Fuchs’ endothelial dystrophy, the most common DMEK indication, and 12 eyes targeted a plano refractive outcome.
STABILISATION BEFORE LOCK-IN
Following DMEK, corneal topography can change due to oedema resolution, Dr Price noted. Therefore, patients had at least three refractions to ensure refractive stability before adjusting the LAL’s power. Most patients had one to two adjustments, with 14% requiring three. Adjustments were made one week apart and locked in once they were within 0.25 D of the target. Patients wore UV-blocking sunglasses until the final lock-in.
Initial vision results are very positive, Dr Price said. For the 12 eyes targeting plano, 92% ended up with 20/20 uncorrected distance visual acuity and 100% with 20/25. Half of the eyes also reached 20/30 near vision uncorrected and 67% 20/40 near vision. Before surgery, just 25% reached 20/20 distance vision corrected.
Residual refractive error was minimal as well, with 93% within 0.25 D sphere and 100% within 0.5 D cylinder after lock-in, Dr Price reported. The results were as good or better than previously reported staged procedures. The study is ongoing for longer follow-up time and additional eyes, he concluded.
i Journal of Cataract & Refractive Surgery. 2015; 41: 1182–9.
David A Price MD is a resident in ophthalmology at Indiana University School of Medicine, Indianapolis, Indiana, USA. price30@iupui.edu
Francis W Price Jr, MD is an ophthalmologist at Price Vision Group, Indianapolis.