Cataract, Refractive, Refractive Surgery
Always Measure the Epithelium!
Epithelium thickness mapping key to better refractive outcomes.

Laura Gaspari
Published: Monday, March 3, 2025
“ What we need is a way of distinguishing which eye that looks normal on topography could be keratoconic. “
Epithelial thickness mapping is the key to determining suitability for refractive surgery. With the advancement of these techniques in modern anterior segment OCT devices, every surgeon should implement epithelial mapping as part of their assessment, reports Dan Reinstein MD, who has studied the epithelium using VHF digital ultrasound since the early 1990s and published multiple peer-reviewed publications on the topic before the release of the first commercially available OCT epithelial map in 2012.
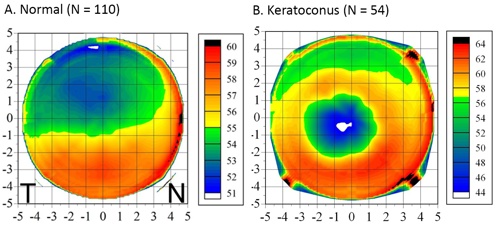
“We know the epithelium is not a single thickness layer, as [previously] thought—it is about 50 μm in the centre,” he said. “It is thicker inferiorly and nasally (Figure 1) due to eyelid dynamics providing an equal and opposite force that maintains the equilibrium of the epithelial cell growth.”
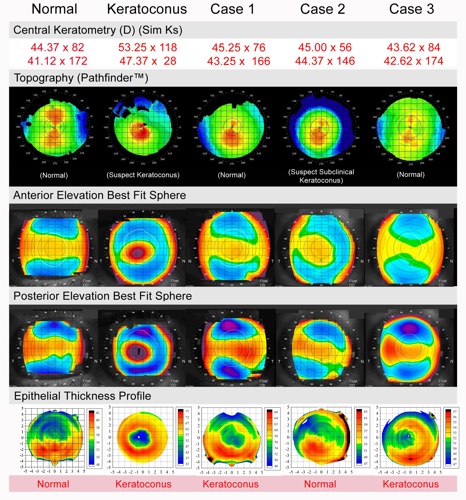
With the advent and development of the OCT, surgeons now have multiple kinds of imaging at their disposal in one device, including the ability to obtain epithelial maps for every patient without obstacles. Regarding suspicious corneas that may appear keratoconic, the epithelium is pivotal to distinguishing whether it is safe to perform refractive surgery. Some patients may have perfectly flat corneas, but the epithelial map demonstrates the eye is keratoconic; conversely, some patients classified as not eligible for surgery due to inferior steepening may have a thick epithelium and can be considered for surgery. (Figure 2) This has enabled ophthalmologists to effectively differentiate between normal and suspicious corneas, improving the safety of refractive surgery.
“What we need is a way of distinguishing which eye that looks normal on topography could be keratoconic,” Professor Reinstein explained.
In the early years of hyperopic LASIK, safety was determined by using parameters focusing solely on keratometry. Prof Reinstein advocates the focus should be on the epithelium instead. There are scenarios after hyperopic LASIK where the keratometry is flat, but the epithelium is thin, meaning an enhancement should not be performed, and vice versa, where an enhancement would be ruled out due to steep keratometry, but the epithelium is still thick.
“Keratometry is a proxy for what you can do with steepening, but it is the wrong number to rely on,” he explained. “The number is the epithelium because the epithelium is what breaks down and can cause repeated trauma and scarring. Being able to distinguish these cases is how you can do safe hyperopic treatments. The epithelial thickness is the actual risk factor, not steepening.”
He added understanding how the epithelium behaves is critical to therapeutic refractive surgery.
“The epithelium thickens to fill any depressions; it thins over the peaks; the change is proportional to the amount of change of stroma, and it is defined by the rate of change of curvature (the curvature gradient).”
This is reflected in the law of epithelial compensation, which states if there is irregular astigmatism, there will be irregular epithelium.
“If an eye presents with irregular topography, the epithelium has reached its maximum compensatory function, leaving irregularity on the surface,” Prof Reinstein explained.
Such presentations bring the possibility of having three identical topographies with three different stromal surfaces, meaning topography measurements can be misleading. “If you have not looked at the epithelium, you cannot judge the corneal irregularity,” he said. “Always measure the epithelium!”
This epithelial compensatory mechanism also enables transepithelial PTK (TE-PTK) to be an extremely effective therapeutic treatment method in cases of irregular astigmatism. TE-PTK uses the epithelium as a natural masking agent to target the ablation onto the peaks on the stromal surface, regularising the stroma.
Prof Reinstein noted these are just some examples of the applications for epithelial thickness mapping that demonstrate how this has become one of, if not the most important, element of diagnostics for refractive surgeons.
Prof Reinstein presented at the 2024 ESCRS Congress in Barcelona.
Dan Zoltan Reinstein MD, MA(Cantab), FRCSC, DABO, FRCOphth, FEBO is a professor of ophthalmology at the London Vision Clinic, UK.
1. Reinstein DZ, Gobbe M, Archer T, Silverman R, Coleman J. “Epithelial, Stromal, and Total Corneal Thickness in Keratoconus,” Journal of Refractive Surgery, 2010 Apr; 26(4): 259–271. Reprint.