Cataract Surgery
Patient Portal
Your questions about Cataract Surgery
A cataract is a misting up of the natural lens, which sits just behind the pupil and helps to focus light on the retina. Cataract surgery involves replacing the misty natural lens with a small, clear synthetic implant called an intraocular lens (IOL). The focusing power of the IOL can be chosen to suit your eye.
IOL implantation is a bit like building your glasses or contact lenses into your eyes. There are three main IOL types:
- Monofocal IOLs – monofocal IOLs aim to reduce spectacle dependence for distance (driving) vision.
- Enhanced monofocal and EDOF IOLs – aim to reduce spectacle dependence for distance and intermediate vision
- Multifocal IOLs – multifocal IOLs aim to reduce spectacle dependence for a wider range of activities, including intermediate (computer screens) and near (reading) vision.
If you are suitable for cataract surgery, we will discuss which IOL type is the best option for you.
Cataracts cause a gradual blurring of your vision and light scatter symptoms such as glare from oncoming car headlights. Your spectacle prescription can also become unstable when you start to develop cataracts. All these problems are normally corrected by cataract surgery.
Cataract surgery can also help you to become less dependent on glasses, particularly if you are suitable for multifocal IOLs.
The visual results of cataract surgery depend on the health of the rest of your eye. Cataracts and some other eye health problems get more common as we get older. So, it is not unusual to have more than one problem with your eye health. If you have an advanced cataract, your lens is sometimes too misty to allow us to examine your eye health fully. At an earlier stage, we are usually able to tell you before your surgery about any additional problems that might affect your visual result, and to advise you on which type of IOL will help you get the best results.
Cataracts can interfere with the monitoring and treatment of eye health problems affecting the back of your eye. Cataract surgery can help facilitate effective care for common eye health problems like glaucoma, diabetic retinopathy, and age-related macular degeneration.
In the absence of a new health problem in the eye, vision normally remains good after cataract surgery. If you do experience any deterioration in vision, it can often be reversed with a one-off minor laser procedure called YAG capsulotomy.
The extent to which cataracts affect your vision is very variable. If you are happy with your vision and still able to do all the things you want to do, there is no need to proceed with treatment. The results of cataract surgery are normally the same, whether the operation is performed at an early stage, or when your cataracts are more advanced.
If you have reached the stage at which blur or light scatter symptoms caused by your cataracts are starting to interfere with your life, perhaps affecting your work, your leisure interests, or your confidence driving, then it makes sense to proceed with treatment.
Although there is never any special urgency, you may choose to proceed with treatment at an early stage. If your main aim is greater spectacle freedom, and you are not yet having any difficulties with your visual quality in glasses or contact lenses, the operation is called refractive lens exchange (RLE). Many people, particularly those with early-stage cataracts, choose this option as an alternative to laser vision correction.
If you are over 50 years of age and have a spectacle prescription higher than the normal range for laser eye surgery, you are likely to be suitable for RLE.
Almost any level of myopia (short sight) or hyperopia (long sight) can be corrected by cataract surgery (RLE), and IOLs with built in astigmatism correction are available. Lens implantation techniques can be combined with laser eye surgery in suitable patients to extend the range of astigmatism treatment or fine-tune the focus outcome.
You may not be suitable for multifocal IOL implantation if you have pre-existing problems with your eye health.
If you are having problems with your vision because of cataracts, they normally get gradually worse with time – although the rate of deterioration is very variable and difficult to predict.
You can choose when you proceed with cataract surgery and delaying treatment will not affect your chances of a good outcome. But cataract surgery is the only effective treatment option.
IOL choices
Different lens implants suit different patients, and not everyone will benefit from multifocal IOL implantation.
Monofocal IOLs may be more suitable if you have other eye problems or if you are worried that you may not cope well with the optical side effects of multifocal IOL implantation. Monofocal IOLs have fewer optical side effects than multifocal IOLs, but do not provide freedom from glasses for such a wide range of activities.
The most commonly used approach in standard cataract surgery is to select monofocal IOLs aiming to leave your eyes equally focused in the distance. Glasses are then usually required for reading and near work.
A common alternative approach using monofocal IOLs is to aim for clearer distance vision in one eye, and clearer vision at arms’ length in the other. With both eyes open, binocular visual input combines to extend the range of focus, improving vision for computer screens and working with your hands. Although you would normally still need glasses for reading, near vision is at least partly restored, with relatively little compromise optically. This spread of binocular focus is sometimes called micromonovision. It can be a good intermediate choice if you would like more freedom from glasses but do not want, or do not have access to, multifocal IOLs.
About 4 out of 5 patients are completely free of glasses after cataract surgery with widely used contemporary (trifocal) multifocal IOLs. If you do need help from glasses after surgery, it is usually for a specific activity in the near, intermediate or distance range. Most people experience some visual side effects from multifocal IOL implantation such as haloes or glare when night driving, but these visual symptoms normally diminish as the visual areas of your brain adapts to the new optical input. Approximately 95% of patients are satisfied with the outcome of surgery, and many describe it as life changing.
Your surgeon may also sometimes recommend ‘extended depth of focus’ (EDOF) or 'enhanced monofocal' IOLs. These are designed as an intermediate option, providing more spectacle freedom than standard monofocal IOLs, and fewer optical side effects than trifocal IOLs.
IOL Options
Toric IOLs are designed to reduce astigmatism. These are available as both multifocal and monofocal IOLs, and they are a good option if your pre-operative tests show that your cornea is ‘more rugby ball shaped than basketball shaped’.
Your surgeon will discuss the pros and cons of different IOL choices in cataract surgery with you at your initial consultation.
Your surgeon will normally perform cataract surgery using local anaesthetic. This may be with drop or gel anaesthetic supplemented by an injection in the back of your hand to relax you if required. Anaesthetic may also be washed around the back of the eye to prevent excessive eye movement. A spring clip holding the eyelids apart allows you to blink safely during surgery.
Your surgeon will be looking through a microscope to perform your surgery. You will be lying down under a surgical tent with fresh air coming in underneath. A sticky plastic drape covers the skin around your eye and sticks the eyelashes out of the way.

Some surgeons now operate on both eyes in sequence on the same day. This helps to get your two eyes working together from day one, accelerating your visual recovery. However, many surgeons prefer to operate on one eye at a time, please do not hesitate to discuss the pros and cons with your surgeon. The surgery typically takes about 20 minutes per eye. You can return home on the same day as surgery.
Strong pupil dilating drugs are given as drops or as a pellet placed under the lower eyelid to prepare your eye for surgery.
Essential steps in cataract surgery are:
- Entry points - formation of small self-sealing entry points in the front of the eye at the junction of the white of the eye and the cornea
- Capsulotomy - removal of a circular disc from the front of the membrane covering the natural lens called the lens capsule (think of the skin of a grape and you will have the right mental image of the thin, clear covering of the natural lens)
- Phacoemulsification – liquefaction and removal of the natural lens from within the lens capsule using a high frequency vibrating probe, fluid washing, and suction pump
- IOL insertion - injection of the IOL and unfolding into the natural position within the lens capsule using a supporting gel to fill the front of the eye
- Wash out and refilling - wash-out of the supporting gel and refilling with fluid and antibiotics.
The steps of cataract surgery
Femtosecond lasers are sometimes now used in a preparatory stage before going through to the operating theatre. Femtosecond lasers are costly and provide no proven benefit for your vision after cataract surgery, but they may make some stages of the operation (capsulotomy in particular) easier for surgeons to perform safely and consistently. This additional laser stage takes about 5 minutes and is performed using eye-drop anaesthetic to numb your eye.
In all forms of eye surgery, problems can occur during the operation or afterwards in the healing period. Problems can result in permanent, serious loss of vision (vision worse than the driving standard in the affected eye that cannot be corrected with glasses or contact lenses). More commonly, problems can be corrected with changes in medication or additional surgery. Typically, these additional operations feel like the original surgery and have a similar recovery period.
Loss of vision
Permanent, serious loss of vision occurs as a result of problems with cataract surgery in approximately 1 in 500 patients. This may mean vision worse than the driving standard or, in some cases, complete loss of vision in the affected eye.
Permanent serious visual loss is typically caused by damage to the retina. This can result from infection or an inflammatory response after surgery, retinal detachment after surgery, or bleeding during surgery. Some problems occurring during surgery increase the risk of sight threatening problems afterwards. These include a common complication of surgery called posterior capsular rupture, (breakage of the membrane just behind the IOL). The rate for capsule rupture for all cataract surgeons is just under 1.5%. For more experienced surgeons it is between 0.5 and 1%. but all surgeons have at least some cases affected by posterior capsular rupture. It is not always possible to implant a multifocal IOL safely if posterior capsular rupture has occurred, and this may mean greater than anticipated reliance on glasses after surgery.
Additional surgery
Second operations may be required to correct a complication from the initial surgery. This could include IOL repositioning or exchange, surgery to retrieve lens fragments from the back of the eye, or retinal detachment repair. With or without cataract surgery, retinal detachments are more common if you are very myopic (short-sighted); but the risk of retinal detachment is approximately five times higher in the first four years after cataract surgery or RLE.
Statistical techniques (biometry formulae) and eye measurements (biometry) are used to guide selection of the IOL required to correct your vision. Limitations on the accuracy of these techniques mean that laser vision correction to fine tune the focus is sometimes required to touch up the visual result after cataract surgery.
The commonest reason for visual deterioration after cataract surgery is posterior capsule opacification (PCO). This is a gradual misting over of the membrane just behind the IOL, which affects many patients. PCO may occur months or years after surgery and is normally treated successfully with a one-off minor laser procedure called YAG laser capsulotomy.
Side effects are problems which most patients experience to some degree after surgery. They normally improve with time, but do not always resolve completely.
Vision
Most patients experience some light scatter side effects and unwanted images in the early months after cataract surgery.
Possible effects on vision
Visual side effects vary with type of IOL implanted and are often more noticeable in some lighting conditions than others. Patients are commonly aware of a shadow or shimmering arc of light in their peripheral vision after monofocal or multifocal IOL implantation. Some types of multifocal IOLs tend to cause halos around lights. Blur or ghost images are more common with others; but almost any form of light scatter side effect can occur, and floaters (floating shadows in your field of vision caused by opacities in the gel filling the back of the eye) may be more apparent after surgery than before – especially in the early period after the operation. It is generally accepted that all forms of multifocal IOL are associated with more optical side effects than monofocal IOLs. However, multifocal IOLs all produce a greater range of spectacle freedom.
Optical side effects may initially interfere with work or leisure activities, and night driving in particular. But they tend to diminish with time. 19 out of 20 patients are satisfied or very satisfied with their vision 3-6 months after multifocal IOL implantation, and laser procedures to treat residual defocus or posterior capsular opacification (YAG capsulotomy for PCO) are often helpful in accelerating adaptation in the remainder. But approximately 1% of patients cannot adapt, and will elect to undergo IOL exchange, a potentially complicated procedure swapping the multifocal IOL for a monofocal IOL. The use of an EDOF or enhanced monofocal IOL may be an alternative at
Eye comfort
Some eye surface discomfort is common in the early months after most forms of eye surgery. This is usually mild after cataract surgery, and highly variable – often affecting one eye more than the other. Treatment and prevention are based on making sure your eye surface is healthy before and after surgery. Lubricant eye drops can be helpful and can be taken safely in addition to your other medication when required. For patients with a normal eye surface prior to surgery, lasting problems are unusual.
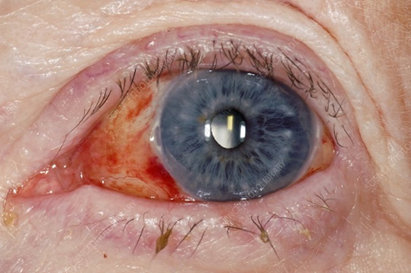
Eye Appearance
Red blotches are often visible on the white of the eye after any form of eye surgery. These are called subconjunctival haemorrhages and are caused by a small leak of blood under the mucous membrane covering the white part of eye wall. Although they can be quite unsightly, red blotches are temporary, and do not affect eye health; but they can take up to 6 weeks to go away completely.
Most IOLs are not visible. But people may occasionally notice a glint in your eye caused by a reflection from the front of the IOL within the pupil.
If you develop a new eye health problem in later life, cataract surgery should not prevent you having successful treatment. Common eye health problems like glaucoma, diabetic retinopathy, and age-related macular degeneration can be monitored and treated as more easily after cataract surgery.
Cataract surgery and RLE create more space for fluid circulation in the front of the eye. This is because IOLs are thinner than the natural lens. This can be beneficial in some types of glaucoma.
If you have hyperopia (long sight), you may have a relatively small space for fluid circulation through the front of the eye – a ‘shallow anterior chamber’, and you may be vulnerable to a form of glaucoma (‘angle closure glaucoma’) caused by blockage of fluid flow that can lead to sudden, painful loss of sight. If you are in this group, cataract surgery (or RLE) both eliminates the risk of angle closure glaucoma and helps you to become less dependent on thick glasses.
Most patients have cataract surgery under local anaesthetic. You can eat and drink normally before surgery and should take any regular medication as usual.
Most surgeons work with an anaesthetist to monitor your health during surgery and optimize your comfort, administering sedation where necessary. Keep your breathing calm, stay as relaxed as you can, and try to keep your head still after the surgeon has positioned it comfortably.
You can help your surgeon apply the drape and stick your eyelashes out of the way by opening both your eyes wide at the beginning of surgery. You should clean off any make-up or moisturising cream before surgery to help the adhesive drape to stick properly. Blinking is no problem after the draping is complete. Just look straight up ahead to the bright operating light with both eyes open, but blink when you need to. Looking up to the bright microscope light helps to keep your eyes in the best position.
Your surgeon will talk you through the procedure, encouraging you at every stage. Let them know if you feel any discomfort, and say if you need to cough, sneeze or take a break.
For the preliminary laser stage in laser assisted cataract surgery, your eye is normally held still and the eyelids are kept out of the way with a suction ring. But the same principles apply. To help the surgery go smoothly, simply stare straight up ahead with both eyes open. Try not to squeeze the eyes shut, but blink whenever you need to.
A clear plastic shield is sometimes taped over the eye at the end of surgery. For most patients, this is no longer required. Non-prescription sunglasses can be worn outdoors whilst the eyes are still a bit light sensitive in the first few days after treatment. You can bring a pair with you on to wear on the way home.
You can wash and shower normally from day one after surgery. Most surgeons recommend no swimming for a week and no contact sports for a month. Non-contact sports such as gym and jogging can be resumed from day one after surgery. It is safe to start driving again when you can read a number plate at 20 metres with both eyes open and you are reasonably comfortable with your new vision. Typically, this is within a few days of surgery.
Set a smart phone reminder and use the antibiotic and anti-inflammatory drops as prescribed to help the eyes to heal well. It is good to leave at least 2 minutes between different types of eye drop so that they each absorb well before the next drop is applied. If you miss the first time or you are not sure, applying a second eye drop is no problem.
Some variability of vision and comfort is normal in the early weeks after cataract surgery, and patience is required. But discomfort is usually mild, and vision normally recovers substantially within 2-3 days once the pupil dilating drugs have worn off.
You should contact your surgeon without delay if you have increasing pain, light sensitivity, redness or blur. You will have been given a telephone number to make contact. If it is out of normal working hours do not hesitate to attend an emergency eye department.
Other danger signs, particularly relevant to highly myopic (short-sighted) patients undergoing cataract surgery, relate to the warning signs of a retinal detachment. These are a sudden new shower of floaters, flashes of light (even with the eyes closed) and visual field loss (a shadow or curtain spreading across your vision). Most retinal detachments can be repaired without detriment to your vision, but the chances of success are much higher if the detachment has not spread across the centre of your vision.
You may not be aware of a problem that requires treatment in the healing phase. So, make sure you attend your review appointments even if your eyes feel good.
Accommodation the reflex by which the eye brings a near object into focus by changing the shape of the natural lens. The natural lens gets less flexible with age, and powers of accommodation diminish. This affects reading vision and the ability to compensate for hyperopia.
Astigmatism irregular defocus, or an eye that is ‘more rugby ball shaped than basketball shaped.’ The first number in your prescription for glasses describes the amount of long or short sight. The second number describes the amount of astigmatism. Most of us have at least some astigmatism, and a small amount can even help extend the range of activities you can do without reading glasses when you get older.
Biometry this test involves measurement of the eye and a set of calculations (biometry formulae) that help determine the right focusing power for an IOL before cataract surgery or RLE.
Binocular vision this is vision measured with the two eyes open.
Cataract when the natural lens gets misty enough to make vision hazy, it is called a cataract.
Cataract surgery this is surgery to replace the natural lens with an IOL. Cataract surgery is identical to RLE but is performed in patients who cannot see clearly despite using glasses or contact lenses with the main aim of restoring clear vision.
Conjunctiva the membrane covering the white of the eye. The conjunctiva produces mucus to help spread the watery tear film over the eye surface.
Cornea the clear part of the eye wall at the front of the eye. Two thirds of the focusing power of the eye is in the cornea.
Corneal epithelium the corneal skin layer
Corneal topography this is a scan that maps the surface curvature of the cornea.
D or Dioptre a unit for measuring the refractive power of a lens.
Excimer laser this type of laser removes tissue by non-thermal vaporisation (photoablation). Excimer lasers are extremely accurate and do not damage the surrounding tissues. They are used in LASIK and surface laser treatments (PRK, LASEK and TransPRK). They may be used to enhance the visual outcome after cataract surgery.
Femtosecond laser this type of laser is designed to cut any 3D shape in clear eye tissues such as the natural lens or the cornea with a high degree of accuracy. They work by creating a 3D pattern of tiny gas bubbles, which is traced through the target tissue at high speed. Femtosecond lasers are used increasingly in RLE and Cataract surgery.
Floaters floating shadows cast on the retina by opacities in the vitreous. Most of us are aware of floaters in some lighting conditions.
Glaucoma this is a condition in which the optic nerve is gradually damaged causing the visual field to contract. Left untreated, patients with glaucoma may develop ‘tunnel vision.’ Glaucoma is often associated with a higher than normal intraocular pressure, and treatment is centred on drugs or surgery to lower the intraocular pressure.
Hyperopia long sight. People with hyperopia typically have good vision as young adults. As they get older, they find themselves reliant on glasses for reading, and then for the distance vision too. Younger people are able to compensate for hyperopia by accommodation. The amount of hyperopia is shown by a positive number in your spectacle prescription.
IOL (intraocular lens) IOLs are small synthetic lens implants that are used to replace the natural lens in cataract surgery and RLE.
Intraocular pressure (IOP) this is the pressure of fluid within the eye. It is often measured with a puff of air in routine eye checks or (more accurately) with a yellow drop and a blue light.
Iris this is the coloured part of the eye behind the cornea that expands and contracts in response to light to dilate or constrict the pupil.
Laser vision correction may be used for correction of sight using excimer and/or femtosecond lasers to alter the curvature and focusing power of the cornea and fine tune vision after cataract surgery.
Meibomian glands the specialized oil glands in the eyelids that pump out a stabilizing layer of oil each time we blink that floats on top of the watery layer of the tear film. Inflammation of the eyelid margins upsetting this layer (blepharitis or meibomitis) is one of the commonest reasons for eye discomfort.
Micromonovision this is the name often given to the strategy of aiming for a clearer distance focus in one eye and a clearer focus at arms’ length in the other. Input from the two eyes combines to extend the range of focus for patients in the reading glasses age group undergoing vision correction surgery.
Monofocal IOL an IOL with one clear point of focus. These are the lenses most commonly used in standard cataract surgery. They have fewer optical side effects than multifocal lenses, but glasses are normally required for at least some activities after implantation.
Multifocal IOL an IOL with more than one point of clear focus This includes enhanced monofocal and Extended Depth of Focus lenses. Multifocal IOLs are often used in RLE in order to help increase freedom from glasses in the near range as well as providing good distance vision.
Myopia short sight. People with myopia are able to see up close but not in the distance. They typically first need glasses as school age children. The amount of myopia is shown as a negative number in your spectacle prescription.
Natural Lens the natural lens sits just behind the pupil and is suspended by a trampoline like array of microligaments from the ciliary muscle, which contracts during accommodation. The natural lens accounts for one third of the focusing power of the eye and is the flexible element of focus. The natural lens gets less flexible with age. It also becomes less clear as we get older. If the natural lens gets misty enough to make vision hazy, it is called a cataract.
Phacoemulsification this is the standard technique for liquefying the natural lens in cataract surgery and RLE. Energy delivered at ultrasonic frequencies from the tip of a fine, hollow probe liquefies the lens. Fluid is washed continuously into the eye around the probe, and the liquefied lens material is sucked away. Where previously the natural lens had to be shelled out like a pea, phacoemulsification allows it to be removed through a tiny, key-hole entry into the eye. This development revolutionised modern cataract surgery. Femtosecond lasers are now commonly used to break the lens up into small fragments before phacoemulsification.
Posterior capsule opacification (PCO) in cataract surgery and RLE, the IOL is implanted within the capsule of the natural lens. This thin, clear membrane then shrink-wraps the IOL and stabilises it in the natural position in the eye. As part of this healing up process, the membrane often goes misty, causing gradual loss of vision after surgery. This is posterior capsule opacification (PCO). It can be treated successfully with a one-off minor laser procedure called YAG capsulotomy.
Presbyopia age related loss of reading vision and the ability to focus on a near object without help from glasses.
Posterior vitreous detachment (PVD) as we age, the vitreous gel shrinks and will often peel off the back of the eye. For some of us, this event passes unnoticed. In others, a new shower of floaters will prompt them to attend for an eye examination. Doctors examining patients after a PVD look carefully for any abnormal attachment of the gel to the retina which could lead to a retinal detachment.
Refraction this is the test that is done to determine the numbers in your spectacle prescription and the amount of myopia, hyperopia or astigmatism.
Refractive surgery this is another name for vision correction surgery or surgery to reduce the need for glasses and contact lenses.
Retina the carpet of light sensitive cells lining the back of the eye, which is sometimes described as ‘the film in the camera.’ Images are focused on the retina by the cornea, the natural lens. Information from the retina is fed through the optic nerve to the visual areas of the brain.
Retinal detachment the retina sometimes detaches from the eye wall and its blood supply. Urgent surgery is then required to re-attach the retina in order to prevent visual loss. Patients with high myopia are more likely to get a retinal detachment. Retinal detachments are also more common in the early years after cataract surgery or RLE. Warning signs are a sudden change in vision with field loss (a dark shadow in part of the visual field); flashing lights (arcs of light – even with the eyes closed); and a sudden new shower of floaters.
RLE (refractive lens exchange) this is surgery to replace the natural lens with an IOL. RLE is identical to cataract surgery but is performed in patients who can see clearly if they wear glasses or contact lenses. The aim of RLE is to help people to see clearly for more activities without glasses or contact lenses.
Tear film a multilayered wet film covering the front of the eye, which is essential for vision and comfort. A layer of mucus produced by specialized cells in the conjunctiva helps the watery layer of the tear film to spread over the eye. The watery layer is stabilized between blinks by an oily layer that forms a thin film (a bit like petrol floating on water) and acts to prevent localized evaporation. The oily layer is pumped out from specialized glands in the eyelids called meibomian glands each time we blink.
Visual acuity this is the main measurement of how well we can see and is tested by asking you to read down a chart which has smaller letters on each line. The lower you can read, the better your visual acuity is. Measurements are expressed as a fraction. If your visual acuity is 6/6 (normal) then you can see at 6 metres what a normally sighted person can see at 6 metres. If your vision is 6/9 you can see at 6 metres what a normally sighted person can see from 9 metres away et cetera. In the USA, the same measurement is made in feet, with 6 metres being roughly 20 feet. Many people are familiar with the American definition of normal ‘20/20’ vision. This is the same as 6/6 vision in the UK measurement.
Vitreous this is the gel filling the back of the eye. It tends to shrink as we age and accumulates wrinkles and opacities that cast floating shadows (floaters) on the retina.
YAG capsulotomy a one-off minor laser procedure used to treat posterior capsule opacification (PCO).