Treating uveitis in children
Many challenges of diagnosis and treatment of paediatric uveitis

Dermot McGrath
Published: Tuesday, October 1, 2019
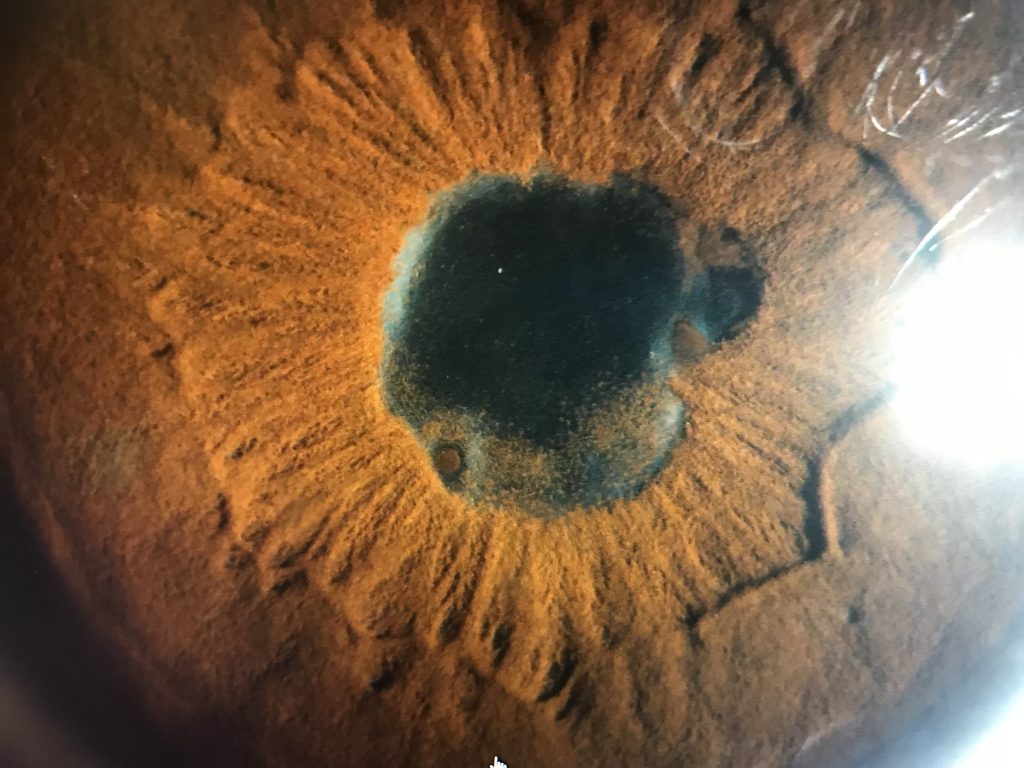 Posterior synechia secondary to HLA B27 anterior uveitis[/caption]
Rapid diagnosis and swift intervention with targeted treatments is essential to reduce the risk of vision-threatening complications in cases of paediatric uveitis, according to Marie-Hélène Errera MD, PhD.
“These cases in children are typically chronic and may result in substantial ocular complications and vision loss if they are not diagnosed and treated appropriately,” she told delegates attending a World Society of Paediatric Ophthalmology and Strabismus (WSPOS) symposium held during the European Society of Ophthalmology (SOE) meeting in Nice, France.
The differential diagnosis of paediatric uveitis is extensive, noted Dr Errera, associate professor of ophthalmology at UPMC Eye Center, Children’s hospital Pittsburgh and at the University of Pittsburgh School of Medicine, Pennsylvania, United States.
As in adult patients, it is important to identify infectious versus non-infectious uveitis as well as anatomic location, since that will have a bearing on prognosis and treatment strategies, she said.
“Of non-infectious causes, juvenile idiopathic arthritis (JIA) is the most common systemic association of paediatric uveitis and accounts for between 35% and 60% of uveitis cases in children,” she said.
Pars planitis is another common idiopathic intermediate uveitis, which predominantly affects children and adolescents, and accounts for up to 28% of paediatric uveitis cases.
“Complications to watch for with pars planitis include cataract, cystoid macular oedema, vitreous opacities, glaucoma, retinoschisis, retinal detachment, epiretinal membrane and optic disc oedema.”
Other autoimmune causes of paediatric uveitis include juvenile sarcoidosis and Blau syndrome, which may also present with joint and eye involvement. Both of these conditions usually present with granulomatous ocular inflammation and can have posterior segment involvement, which is not normally found in JIA-related uveitis, she added.
Posterior synechia secondary to HLA B27 anterior uveitis[/caption]
Rapid diagnosis and swift intervention with targeted treatments is essential to reduce the risk of vision-threatening complications in cases of paediatric uveitis, according to Marie-Hélène Errera MD, PhD.
“These cases in children are typically chronic and may result in substantial ocular complications and vision loss if they are not diagnosed and treated appropriately,” she told delegates attending a World Society of Paediatric Ophthalmology and Strabismus (WSPOS) symposium held during the European Society of Ophthalmology (SOE) meeting in Nice, France.
The differential diagnosis of paediatric uveitis is extensive, noted Dr Errera, associate professor of ophthalmology at UPMC Eye Center, Children’s hospital Pittsburgh and at the University of Pittsburgh School of Medicine, Pennsylvania, United States.
As in adult patients, it is important to identify infectious versus non-infectious uveitis as well as anatomic location, since that will have a bearing on prognosis and treatment strategies, she said.
“Of non-infectious causes, juvenile idiopathic arthritis (JIA) is the most common systemic association of paediatric uveitis and accounts for between 35% and 60% of uveitis cases in children,” she said.
Pars planitis is another common idiopathic intermediate uveitis, which predominantly affects children and adolescents, and accounts for up to 28% of paediatric uveitis cases.
“Complications to watch for with pars planitis include cataract, cystoid macular oedema, vitreous opacities, glaucoma, retinoschisis, retinal detachment, epiretinal membrane and optic disc oedema.”
Other autoimmune causes of paediatric uveitis include juvenile sarcoidosis and Blau syndrome, which may also present with joint and eye involvement. Both of these conditions usually present with granulomatous ocular inflammation and can have posterior segment involvement, which is not normally found in JIA-related uveitis, she added.
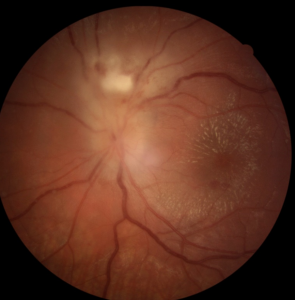 Juxtapapillary retinochoroiditis and macular star
related to toxoplasmosis in a 12-year-old child
Juxtapapillary retinochoroiditis and macular star
related to toxoplasmosis in a 12-year-old child