Negative dysphotopsia
Optical modelling applied to elucidate the cause of bothersome visual symptoms.

Cheryl Guttman Krader
Published: Sunday, March 1, 2020
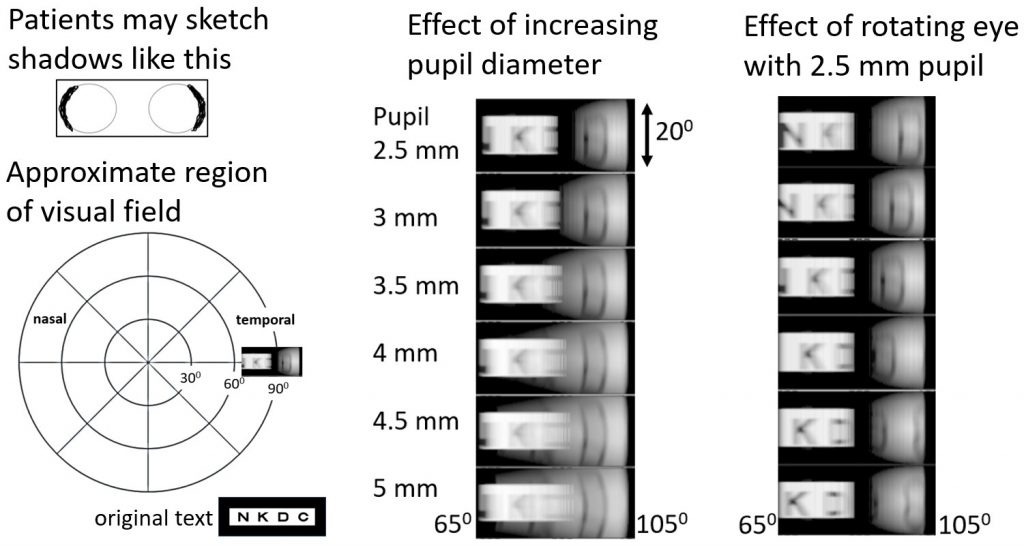 Simulated images of a peripheral region of the visual field for a pseudophakic eye with a 2.5mm diameter pupil. Visual angles are only very approximate. Image courtesy of Michael J Simpson PhD
Researchers appear to have moved towards a hypothesis that explains the cause for negative dysphotopsia, the dark shadows that are perceived in the temporal visual field by some pseudophakic patients.
Confirmation of the hypothesis, however, requires further study to fill gaps in data for a variety of related parameters, said Michael J Simpson PhD.
Speaking at the 37th Congress of the ESCRS in Paris, France, Dr Simpson discussed optical modelling work he has been doing with ray tracing to understand far peripheral vision and to characterise the aetiology of negative dysphotopsia. Dr Simpson is an optics expert from Arlington, TX, USA.
He told attendees that while negative dysphotopsia has been considered an artefact associated with certain IOLs or surgical techniques, it is probably actually a fundamental property of the optics of the pseudophakic eye (Figure 1).
“In the phakic eye, the crystalline lens pushes the iris forward, and all light passing through the pupil enters the lens and forms an image. With an IOL, however, the lens is very much smaller, and there is also a gap between the iris and lens. The result of these differences is that at large visual angles the main image goes dark because light no longer enters the lens, and a shadow region is created in the periphery,” Dr Simpson said.
“Light that misses the lens illuminates the shadow as the pupil opens so that the shadow rapidly disappears. This sensitivity to pupil size may explain why negative dysphotopsia can be so bothersome to patients.”
This explanation for the cause of negative dysphotopsia is consistent with patient complaints, which only arose after small incision surgery using phacoemulsification and foldable IOLs improved capsule clarity, which probably provided a direct path to the peripheral retina, Dr Simpson said.
Modelling research
Because the pseudophakic eye is an unusual imaging system, the ray-tracing calculations for studying negative dysphotopsia uses special calculations with the Zemax optical design software. In addition, Dr Simpson has used simulated text rather than just a uniformly bright object field to gain a better understanding of far peripheral vision (Figure 2).
The results from the modelling showed that light missing the IOL comes from a lower visual angle and experiences lower power so that it forms a larger image. The research also demonstrated the effect of pupil size on negative dysphotopsia as well as the potential that different lens styles may have different effects. In addition, it has provided information about how the IOL haptic junction can affect negative dysphotopsia and the changes that occur with sulcus implantation of a piggyback IOL.
“Whereas earlier discussions indicated that the cause of negative dysphotopsia was unknown, patients are likely to be reassured if told that the dark shadows they are seeing have a known cause. Although sulcus implantation of a piggyback IOL may be effective sometimes in reducing or eliminating negative dysphotopsia, the new evaluations may help with management of the issue.”
Future directions
Dr Simpson stated that there is a basic need to improve characterisation of vision in the far periphery, which is largely a neglected topic. There is also a need for more clinical data relating to negative dysphotopsia.
“According to the literature, negative dysphotopsia seems to be mainly visible when the pupil is small. We need to know at what visual angle and at what pupil diameters the shadow becomes bothersome for patients, and studies should not group together multiple lens styles,” Dr Simpson said.
Perimetry is the main test that is used to measure peripheral vision in general, but typically pupil diameter is neither controlled nor measured, and there is no mechanism for dealing with a peripheral double image.
“With complete patient data and optical modelling, we should be able to verify the cause of negative dysphotopsia and understand why only some patients complain about this symptom. This new knowledge is then likely to lead to longer term solutions,” Dr Simpson said. The current work has been accepted for publication by the Journal of Cataract & Refractive Surgery (JCRS).
Michael J Simpson: mjs1@outlook.com
Simulated images of a peripheral region of the visual field for a pseudophakic eye with a 2.5mm diameter pupil. Visual angles are only very approximate. Image courtesy of Michael J Simpson PhD
Researchers appear to have moved towards a hypothesis that explains the cause for negative dysphotopsia, the dark shadows that are perceived in the temporal visual field by some pseudophakic patients.
Confirmation of the hypothesis, however, requires further study to fill gaps in data for a variety of related parameters, said Michael J Simpson PhD.
Speaking at the 37th Congress of the ESCRS in Paris, France, Dr Simpson discussed optical modelling work he has been doing with ray tracing to understand far peripheral vision and to characterise the aetiology of negative dysphotopsia. Dr Simpson is an optics expert from Arlington, TX, USA.
He told attendees that while negative dysphotopsia has been considered an artefact associated with certain IOLs or surgical techniques, it is probably actually a fundamental property of the optics of the pseudophakic eye (Figure 1).
“In the phakic eye, the crystalline lens pushes the iris forward, and all light passing through the pupil enters the lens and forms an image. With an IOL, however, the lens is very much smaller, and there is also a gap between the iris and lens. The result of these differences is that at large visual angles the main image goes dark because light no longer enters the lens, and a shadow region is created in the periphery,” Dr Simpson said.
“Light that misses the lens illuminates the shadow as the pupil opens so that the shadow rapidly disappears. This sensitivity to pupil size may explain why negative dysphotopsia can be so bothersome to patients.”
This explanation for the cause of negative dysphotopsia is consistent with patient complaints, which only arose after small incision surgery using phacoemulsification and foldable IOLs improved capsule clarity, which probably provided a direct path to the peripheral retina, Dr Simpson said.
Modelling research
Because the pseudophakic eye is an unusual imaging system, the ray-tracing calculations for studying negative dysphotopsia uses special calculations with the Zemax optical design software. In addition, Dr Simpson has used simulated text rather than just a uniformly bright object field to gain a better understanding of far peripheral vision (Figure 2).
The results from the modelling showed that light missing the IOL comes from a lower visual angle and experiences lower power so that it forms a larger image. The research also demonstrated the effect of pupil size on negative dysphotopsia as well as the potential that different lens styles may have different effects. In addition, it has provided information about how the IOL haptic junction can affect negative dysphotopsia and the changes that occur with sulcus implantation of a piggyback IOL.
“Whereas earlier discussions indicated that the cause of negative dysphotopsia was unknown, patients are likely to be reassured if told that the dark shadows they are seeing have a known cause. Although sulcus implantation of a piggyback IOL may be effective sometimes in reducing or eliminating negative dysphotopsia, the new evaluations may help with management of the issue.”
Future directions
Dr Simpson stated that there is a basic need to improve characterisation of vision in the far periphery, which is largely a neglected topic. There is also a need for more clinical data relating to negative dysphotopsia.
“According to the literature, negative dysphotopsia seems to be mainly visible when the pupil is small. We need to know at what visual angle and at what pupil diameters the shadow becomes bothersome for patients, and studies should not group together multiple lens styles,” Dr Simpson said.
Perimetry is the main test that is used to measure peripheral vision in general, but typically pupil diameter is neither controlled nor measured, and there is no mechanism for dealing with a peripheral double image.
“With complete patient data and optical modelling, we should be able to verify the cause of negative dysphotopsia and understand why only some patients complain about this symptom. This new knowledge is then likely to lead to longer term solutions,” Dr Simpson said. The current work has been accepted for publication by the Journal of Cataract & Refractive Surgery (JCRS).
Michael J Simpson: mjs1@outlook.com