Limbal deficiency
Studies give insight on the best technique for transplantation with limbal stem cells

Cheryl Guttman Krader
Published: Tuesday, July 9, 2019
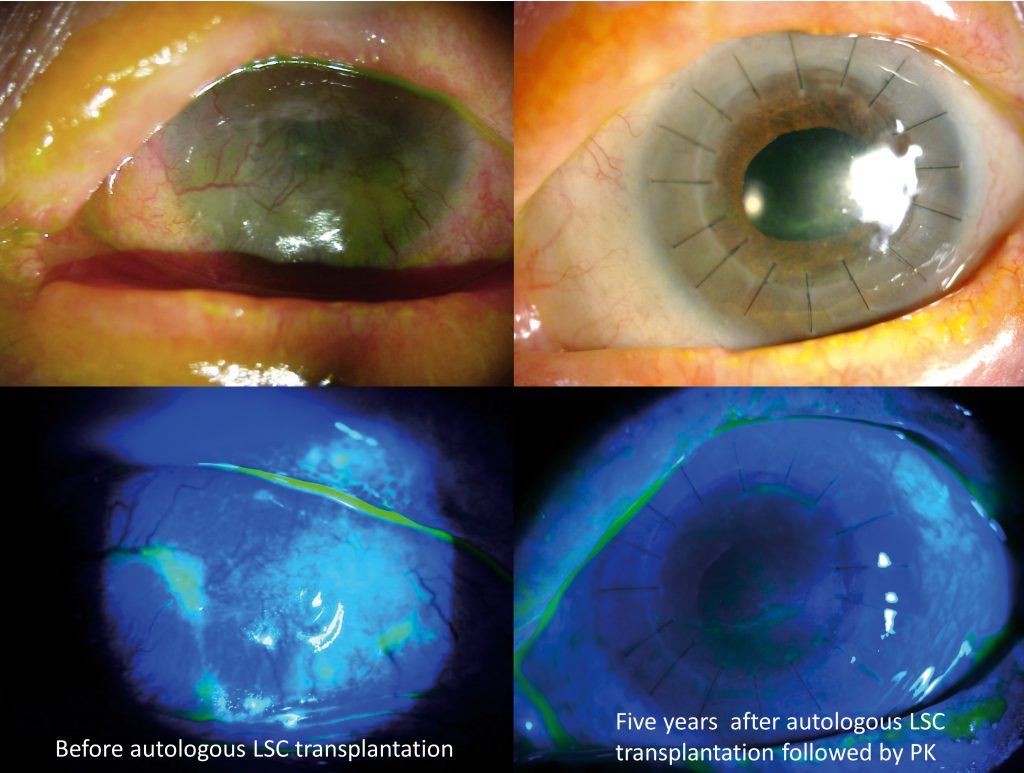 Image courtesy of Vincent M Borderie MD, PhD
Outcomes from long-term follow-up of patients treated for stage 3 limbal deficiency favour a transplantation approach that uses cultured autologous limbal stem cells (LSCs) rather than cultured allogeneic cells or limbal tissue transplantation.
At the 2019 meeting of the Association for Research in Vision and Ophthalmology (ARVO) in Vancouver, Canada, Vincent M Borderie MD, PhD, presented findings from two studies – a phase II prospective trial comparing the efficiency and safety of transplantation of autologous and allogeneic LSCs cultured on human amniotic membrane with no feeders, and a retrospective study of patients who received allogeneic or autologous limbal tissue transplants.
He reported that the cultured autologous LSC transplant was associated with the best graft survival, safety profile and vision improvement, and the long-term survival rate was also similar to that reported in published large studies evaluating transplantation of cultured autologous LSCs.
Autologous limbal grafts had good survival but lower safety than the cultured autologous LSCs. Grafts using allogeneic cultured LSCs or limbal tissue were associated with a low long-term success rate and a high rate of serious adverse events.
“Currently, we have several therapeutic approaches that can be used to treat advanced LSC deficiency, but we are missing studies that compare the different techniques to help us determine which would be best for a given patient,” said Dr Borderie, Professor and Chairman, Department of Ophthalmology, University Paris VI Pierre & Marie Curie, Paris, France.
All of the patients enrolled in the prospective study had stage 3 limbal deficiency with superficial vascularisation and late fluorescein staining, and they had poor visual acuity (VA; 20/200 or worse).
Following transplantation, regardless of the type of graft received, all patients were treated with topical corticosteroids and artificial tears. Additional therapies included autologous serum eye drops for patients who received cultured LSC transplants, topical cyclosporine for those who received allogenic stem cells and one year of systemic immunosuppression for patients who received allogeneic cultured LSC transplants.
“We hypothesised that we would have less rejection and therefore avoid the need for systemic immunosuppression after transplantation of the allogeneic cultured LSC graft compared to LSC transplantation because we thought that we would avoid having immune cells in the cultured graft. However, the allogeneic tissue and cultured cell grafts behaved the same way,” Dr Borderie said.
STUDY RESULTS
The estimated five-year survival rate was 71% for the autologous cultured LSCs and 75% for the autologous limbal transplant. The difference between groups was not statistically significant. Five-year survival was only 33% for the allogeneic limbal transplant and 0% in the allogeneic cultured LSC group.
Visual acuity improved only in patients who received an autologous transplant, and declined in the allogeneic transplant groups. In the autologous groups, the mean improvement was higher in patients who received the cultured LSC transplants than in the limbal tissue group (+9.2 vs +3.3 lines).
Other assessments showed that subjective symptoms improved after transplantation of the cultured autologous LSCs, and eyes treated with this technique had a significant reduction in fluorescein staining. The area of the cornea that
was free of superficial vessels also increased significantly in the cultured autologous LSC group compared with both baseline and the change observed in the allogeneic LSC group. Fluorescein staining increased after transplantation of the allogeneic LSC transplant.
Dr Borderie also reported that compared with failed grafts, the successful grafts had a greater decrease in fluorescein staining from baseline, a greater vascularisation-free area in the superficial cornea, lower variability of corneal epithelial thickness and higher corneal epithelial basal cell density.
SAFETY REVIEW
Dr Borderie observed there were “major” differences in safety between groups.
“Adverse events occurred at a low frequency and were minor in the group that had transplantation with autologous cultured LSCs. Patients who had autologous limbal tissue transplantation were more likely to experience adverse events, some of which were sight-threatening. Patients who got allogeneic stem cells had a high-frequency of sight-threatening adverse events,” he said.
Vincent Borderie: Vincent.borderie@upmc.fr
Image courtesy of Vincent M Borderie MD, PhD
Outcomes from long-term follow-up of patients treated for stage 3 limbal deficiency favour a transplantation approach that uses cultured autologous limbal stem cells (LSCs) rather than cultured allogeneic cells or limbal tissue transplantation.
At the 2019 meeting of the Association for Research in Vision and Ophthalmology (ARVO) in Vancouver, Canada, Vincent M Borderie MD, PhD, presented findings from two studies – a phase II prospective trial comparing the efficiency and safety of transplantation of autologous and allogeneic LSCs cultured on human amniotic membrane with no feeders, and a retrospective study of patients who received allogeneic or autologous limbal tissue transplants.
He reported that the cultured autologous LSC transplant was associated with the best graft survival, safety profile and vision improvement, and the long-term survival rate was also similar to that reported in published large studies evaluating transplantation of cultured autologous LSCs.
Autologous limbal grafts had good survival but lower safety than the cultured autologous LSCs. Grafts using allogeneic cultured LSCs or limbal tissue were associated with a low long-term success rate and a high rate of serious adverse events.
“Currently, we have several therapeutic approaches that can be used to treat advanced LSC deficiency, but we are missing studies that compare the different techniques to help us determine which would be best for a given patient,” said Dr Borderie, Professor and Chairman, Department of Ophthalmology, University Paris VI Pierre & Marie Curie, Paris, France.
All of the patients enrolled in the prospective study had stage 3 limbal deficiency with superficial vascularisation and late fluorescein staining, and they had poor visual acuity (VA; 20/200 or worse).
Following transplantation, regardless of the type of graft received, all patients were treated with topical corticosteroids and artificial tears. Additional therapies included autologous serum eye drops for patients who received cultured LSC transplants, topical cyclosporine for those who received allogenic stem cells and one year of systemic immunosuppression for patients who received allogeneic cultured LSC transplants.
“We hypothesised that we would have less rejection and therefore avoid the need for systemic immunosuppression after transplantation of the allogeneic cultured LSC graft compared to LSC transplantation because we thought that we would avoid having immune cells in the cultured graft. However, the allogeneic tissue and cultured cell grafts behaved the same way,” Dr Borderie said.
STUDY RESULTS
The estimated five-year survival rate was 71% for the autologous cultured LSCs and 75% for the autologous limbal transplant. The difference between groups was not statistically significant. Five-year survival was only 33% for the allogeneic limbal transplant and 0% in the allogeneic cultured LSC group.
Visual acuity improved only in patients who received an autologous transplant, and declined in the allogeneic transplant groups. In the autologous groups, the mean improvement was higher in patients who received the cultured LSC transplants than in the limbal tissue group (+9.2 vs +3.3 lines).
Other assessments showed that subjective symptoms improved after transplantation of the cultured autologous LSCs, and eyes treated with this technique had a significant reduction in fluorescein staining. The area of the cornea that
was free of superficial vessels also increased significantly in the cultured autologous LSC group compared with both baseline and the change observed in the allogeneic LSC group. Fluorescein staining increased after transplantation of the allogeneic LSC transplant.
Dr Borderie also reported that compared with failed grafts, the successful grafts had a greater decrease in fluorescein staining from baseline, a greater vascularisation-free area in the superficial cornea, lower variability of corneal epithelial thickness and higher corneal epithelial basal cell density.
SAFETY REVIEW
Dr Borderie observed there were “major” differences in safety between groups.
“Adverse events occurred at a low frequency and were minor in the group that had transplantation with autologous cultured LSCs. Patients who had autologous limbal tissue transplantation were more likely to experience adverse events, some of which were sight-threatening. Patients who got allogeneic stem cells had a high-frequency of sight-threatening adverse events,” he said.
Vincent Borderie: Vincent.borderie@upmc.fr