Imaging in cataract & refractive surgery
There are a range of options available for the assesment and measurement of the anterior segment.

Soosan Jacob
Published: Tuesday, October 1, 2019
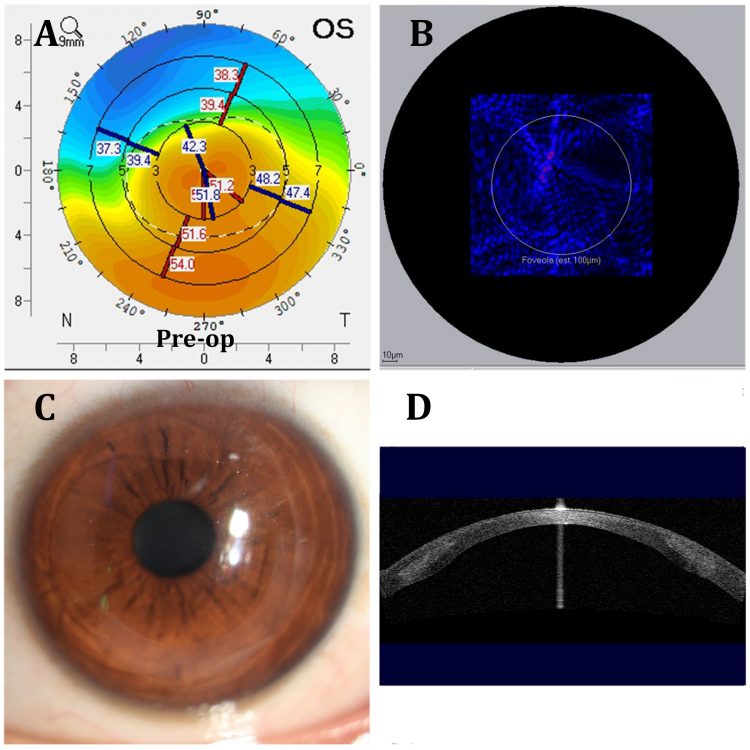 Use of imaging in keratoconus: A,B: Preoperative evaluation – axial curvature map on the Pentacam® (A); Point Spread function seen on Zywave® aberrometry map (B); C: Slit-lamp photography showing cornea after CAIRS (Corneal Allogenic Intrastromal Ring Segments) implantation; D: ASOCT image showing CAIRS segments in situ
Unlike physicians who often have to take educated guesses to formulate even a provisional diagnosis, ophthalmologists are blessed in having a transparent cornea that allows direct visualisation of pathology preoperatively and the actual surgical field postoperatively. However, there are still situations where we, like our medical and surgical counterparts, have to depend on other modalities for additional information. This article deals with anterior segment imaging in cataract and refractive surgery.
Anterior segment optical coherence tomography (ASOCT)
Described in 2000, OCT can be used to image ocular tissues right from cornea to retina. Dedicated anterior segment units, combined units as well as posterior segment units with accessories that allow anterior segment scanning are available.
OCT may be time domain, spectral domain or swept source – the latter two take up to 100,000 scans/second with resolution of 1-10 microns. Imaging is based on grade of tissue opacity. Ciliary body and retro-iridal structures, however, cannot be imaged.
Advantages include fast scanning, high resolution, wide applicability and non-contact testing. Linear scans, raster scans, three-dimensional scans and pachymetric maps are obtained.
ASOCT has numerous uses – pachymetric and epithelial thickness maps can help decide for or against refractive surgery in patients with suspicious topography. Depth of scars is assessed
for performing phototherapeutic keratectomy or for deciding between LASIK and photorefractive keratectomy. LASIK flap thickness and residual bed thickness help decision-making in enhancement surgeries.
The LASIK flap, SMILE® cap, any interface debris, epithelial ingrowth, infiltrates, fluid collection etc. can all be analysed. OCT is also useful for post-surgical evaluation of anterior and posterior chamber phakic IOLs.
In glaucoma, it helps assess angle anatomy, occludability, physiological changes to light/medication or accommodation, diagnosis of narrow angles and plateau iris, assessment of post-laser or post-surgical changes, postoperative bleb morphology, position of tubes, shunts and MIGS devices. Prior to premium IOL implantation, posterior segment OCT helps rule out macular pathology. ASOCT also helps postoperatively in diagnosing Descemet’s detachments, IOL position, tilt, centration, assessment of zonulopathy, posterior capsular opacification etc.
Ultrasound biomicroscopy (UBM)
Invented in 1990, this uses B-scan mode ultrasonography, has tissue penetration of about 5mm and resolution of 25 microns. It is extremely useful when retro-iridal and sulcal areas, zonules, periphery of capsular bag, IOL haptics and ciliary body need imaging. It can also be used to assess angle and other anterior segment structures. However, an immersion technique, need for an experienced examiner, supine position testing, changes in angle anatomy in supine position etc are disadvantages.
Topography and tomography
Topographic devices assess only the anterior corneal surface whereas tomographic devices such as Pentacam® (Oculus Inc), Orbscan® (B&L), Sirius® (CSO) and Galilei® (Zeimer) assess anterior and posterior corneal surfaces, anterior chamber, iris and lens. These are invaluable for patient assessment before cornea- and lens-based refractive surgeries such as SMILE, LASIK and phakic IOL.
They help in screening; planning of refractive surgery; evaluation of post-refractive surgery patient; evaluation and treatment of keratoconus, post-LASIK ectasia, irregular corneas, corneal scars, corneal transplants etc.
They are used for planning Intra Corneal Ring Segments as well as CAIRS (Corneal Allogenic Intrastromal Ring Segments) implantation in patients with keratoconus. Difference maps are used for evaluating progression or treatment effect. Phakic IOL software in Pentacam® can simulate lens position preoperatively.
For cataract surgery, net corneal power can be measured to calculate IOL power in patients with previous corneal surgery. Axial length may be measured by Pentacam® AXL and used for IOL power calculation with inbuilt software.
Toric IOL planning, assessment of posterior corneal astigmatism, measurement of corneal higher- and lower-order aberrations including spherical aberration, grading of lens opacity and lens thickness before cataract surgery are all possible.
Pentacam®, Cassini® (i-Optics), OPD-Scan III® (Nidek), Aladdin® (Topcon) can all be integrated with the Lensar® femtosecond laser cataract platform to accurately perform arcuate incisions and to create anterior capsular nubs for toric IOL alignment. Corrected IOP measurements, corneal white to white, pupil size and angle kappa, densitometry values for lens and cornea, glaucoma screening – evaluation of angle and anterior chamber anatomy are other features. Topolyzer® (Alcon) gives Zernicke and Fourier analysis and pupil centroid shift and is used for topography-guided LASIK.
Scheimpflug imaging is also used by Corvis® ST (Oculus) to record corneal reaction to a defined air pulse to measure IOP, pachymetry and biomechanical corrected IOP. Corvis Biomechanical Index and Tomographic Biomechanical Index (with Pentacam) are also calculated.
Slit-lamp photography
This is becoming popular as tele-ophthalmology takes root. Choices include high-end slit-lamp integrated cameras with dedicated software or simple mobile phone camera fixed to the ocular of any slit-lamp via an adapter to click images that can then be transmitted via internet.
Epithelial mapping
Detailed measurements of corneal epithelium over the entire cornea are presented as epithelial maps that help analyse and differentiate between pseudo- and true form fruste keratoconus and to detect sub-clinical keratoconus in patients with apparently normal topographic maps. It is a useful tool for refractive surgery candidates, patients with keratoconus and other causes of irregular corneas. It helps understand epithelial remodelling as a cause for post-LASIK regression and helps plan any corrective refractive surgery. Mapping may be done using OCT RTVue® (Optovue) or very high-frequency (VHF) digital ultrasound Artemis® (ArcScan).
Wavefront imaging
Aberrometers measure the wavefront of the eye, map them and give an assessment of higher- and lower-order aberrations. They measure total eye aberrations and help in separating lenticular from corneal aberrations. They are useful in assessing refractive surgery candidates, planning wavefront-guided LASIK and for evaluating keratoconus and other causes of irregular corneas.
Premium IOLs may cause visual dissatisfaction in patients with irregular or post-refractive surgery corneas and preoperative aberrometry is useful to avoid such situations. Intraoperative aberrometry is also possible and helps in IOL power selection, toric IOL selection and placement, placing limbal-relaxing incisions etc and is especially useful in post-refractive surgery patients. Software can help compare pre-, intra- and postoperative data to allow constant improvement.
Tear film imaging and Meibography
OCT, fringe interferometry and other techniques are used to image the tear film and its layers. This is useful for diagnosis and management of dry eye disease. Tear meniscus height, non-invasive tear break-up time and blink rate can also be measured. Meibography uses infrared illumination to evaluate Meibomian gland function, density and anatomy as well as capture images for patient education and documentation.
In vitro confocal microscopy
(IVCM)
Microscopic imaging of living cornea by IVCM without damaging tissue is used to diagnose Acanthamoeba keratitis, keratoconus, dry eyes etc, and to monitor response to therapy and surgery.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India and can be reached at dr_soosanj@hotmail.com
Use of imaging in keratoconus: A,B: Preoperative evaluation – axial curvature map on the Pentacam® (A); Point Spread function seen on Zywave® aberrometry map (B); C: Slit-lamp photography showing cornea after CAIRS (Corneal Allogenic Intrastromal Ring Segments) implantation; D: ASOCT image showing CAIRS segments in situ
Unlike physicians who often have to take educated guesses to formulate even a provisional diagnosis, ophthalmologists are blessed in having a transparent cornea that allows direct visualisation of pathology preoperatively and the actual surgical field postoperatively. However, there are still situations where we, like our medical and surgical counterparts, have to depend on other modalities for additional information. This article deals with anterior segment imaging in cataract and refractive surgery.
Anterior segment optical coherence tomography (ASOCT)
Described in 2000, OCT can be used to image ocular tissues right from cornea to retina. Dedicated anterior segment units, combined units as well as posterior segment units with accessories that allow anterior segment scanning are available.
OCT may be time domain, spectral domain or swept source – the latter two take up to 100,000 scans/second with resolution of 1-10 microns. Imaging is based on grade of tissue opacity. Ciliary body and retro-iridal structures, however, cannot be imaged.
Advantages include fast scanning, high resolution, wide applicability and non-contact testing. Linear scans, raster scans, three-dimensional scans and pachymetric maps are obtained.
ASOCT has numerous uses – pachymetric and epithelial thickness maps can help decide for or against refractive surgery in patients with suspicious topography. Depth of scars is assessed
for performing phototherapeutic keratectomy or for deciding between LASIK and photorefractive keratectomy. LASIK flap thickness and residual bed thickness help decision-making in enhancement surgeries.
The LASIK flap, SMILE® cap, any interface debris, epithelial ingrowth, infiltrates, fluid collection etc. can all be analysed. OCT is also useful for post-surgical evaluation of anterior and posterior chamber phakic IOLs.
In glaucoma, it helps assess angle anatomy, occludability, physiological changes to light/medication or accommodation, diagnosis of narrow angles and plateau iris, assessment of post-laser or post-surgical changes, postoperative bleb morphology, position of tubes, shunts and MIGS devices. Prior to premium IOL implantation, posterior segment OCT helps rule out macular pathology. ASOCT also helps postoperatively in diagnosing Descemet’s detachments, IOL position, tilt, centration, assessment of zonulopathy, posterior capsular opacification etc.
Ultrasound biomicroscopy (UBM)
Invented in 1990, this uses B-scan mode ultrasonography, has tissue penetration of about 5mm and resolution of 25 microns. It is extremely useful when retro-iridal and sulcal areas, zonules, periphery of capsular bag, IOL haptics and ciliary body need imaging. It can also be used to assess angle and other anterior segment structures. However, an immersion technique, need for an experienced examiner, supine position testing, changes in angle anatomy in supine position etc are disadvantages.
Topography and tomography
Topographic devices assess only the anterior corneal surface whereas tomographic devices such as Pentacam® (Oculus Inc), Orbscan® (B&L), Sirius® (CSO) and Galilei® (Zeimer) assess anterior and posterior corneal surfaces, anterior chamber, iris and lens. These are invaluable for patient assessment before cornea- and lens-based refractive surgeries such as SMILE, LASIK and phakic IOL.
They help in screening; planning of refractive surgery; evaluation of post-refractive surgery patient; evaluation and treatment of keratoconus, post-LASIK ectasia, irregular corneas, corneal scars, corneal transplants etc.
They are used for planning Intra Corneal Ring Segments as well as CAIRS (Corneal Allogenic Intrastromal Ring Segments) implantation in patients with keratoconus. Difference maps are used for evaluating progression or treatment effect. Phakic IOL software in Pentacam® can simulate lens position preoperatively.
For cataract surgery, net corneal power can be measured to calculate IOL power in patients with previous corneal surgery. Axial length may be measured by Pentacam® AXL and used for IOL power calculation with inbuilt software.
Toric IOL planning, assessment of posterior corneal astigmatism, measurement of corneal higher- and lower-order aberrations including spherical aberration, grading of lens opacity and lens thickness before cataract surgery are all possible.
Pentacam®, Cassini® (i-Optics), OPD-Scan III® (Nidek), Aladdin® (Topcon) can all be integrated with the Lensar® femtosecond laser cataract platform to accurately perform arcuate incisions and to create anterior capsular nubs for toric IOL alignment. Corrected IOP measurements, corneal white to white, pupil size and angle kappa, densitometry values for lens and cornea, glaucoma screening – evaluation of angle and anterior chamber anatomy are other features. Topolyzer® (Alcon) gives Zernicke and Fourier analysis and pupil centroid shift and is used for topography-guided LASIK.
Scheimpflug imaging is also used by Corvis® ST (Oculus) to record corneal reaction to a defined air pulse to measure IOP, pachymetry and biomechanical corrected IOP. Corvis Biomechanical Index and Tomographic Biomechanical Index (with Pentacam) are also calculated.
Slit-lamp photography
This is becoming popular as tele-ophthalmology takes root. Choices include high-end slit-lamp integrated cameras with dedicated software or simple mobile phone camera fixed to the ocular of any slit-lamp via an adapter to click images that can then be transmitted via internet.
Epithelial mapping
Detailed measurements of corneal epithelium over the entire cornea are presented as epithelial maps that help analyse and differentiate between pseudo- and true form fruste keratoconus and to detect sub-clinical keratoconus in patients with apparently normal topographic maps. It is a useful tool for refractive surgery candidates, patients with keratoconus and other causes of irregular corneas. It helps understand epithelial remodelling as a cause for post-LASIK regression and helps plan any corrective refractive surgery. Mapping may be done using OCT RTVue® (Optovue) or very high-frequency (VHF) digital ultrasound Artemis® (ArcScan).
Wavefront imaging
Aberrometers measure the wavefront of the eye, map them and give an assessment of higher- and lower-order aberrations. They measure total eye aberrations and help in separating lenticular from corneal aberrations. They are useful in assessing refractive surgery candidates, planning wavefront-guided LASIK and for evaluating keratoconus and other causes of irregular corneas.
Premium IOLs may cause visual dissatisfaction in patients with irregular or post-refractive surgery corneas and preoperative aberrometry is useful to avoid such situations. Intraoperative aberrometry is also possible and helps in IOL power selection, toric IOL selection and placement, placing limbal-relaxing incisions etc and is especially useful in post-refractive surgery patients. Software can help compare pre-, intra- and postoperative data to allow constant improvement.
Tear film imaging and Meibography
OCT, fringe interferometry and other techniques are used to image the tear film and its layers. This is useful for diagnosis and management of dry eye disease. Tear meniscus height, non-invasive tear break-up time and blink rate can also be measured. Meibography uses infrared illumination to evaluate Meibomian gland function, density and anatomy as well as capture images for patient education and documentation.
In vitro confocal microscopy
(IVCM)
Microscopic imaging of living cornea by IVCM without damaging tissue is used to diagnose Acanthamoeba keratitis, keratoconus, dry eyes etc, and to monitor response to therapy and surgery.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India and can be reached at dr_soosanj@hotmail.com
Tags: cataract and refractive surgery, imaging
Latest Articles
Beyond the Numbers
Empowering patient participation fosters continuous innovation in cataract surgery.
Thinking Beyond the Surgery Room
Practice management workshop focuses on financial operations and AI business applications.
Aid Cuts Threaten Global Eye Care Progress
USAID closure leads retreat in development assistance.
Supplement: ESCRS Clinical Trends Series: Presbyopia
Debate: FS-LASIK or KLEx for Hyperopia?
FS-LASIK has more of a track record, but KLEx offers advantages.
Four AI Applications Ready for Practice
Commercial offerings may save time, improve practice and research.
Perioperative Medication Regimens for Cataract Surgery
Randomised controlled clinical trial results provide evidence-based guidance.
Should Fuchs’ Dystrophy Patients Get Premium Lenses?
Patients’ demand for premium IOLs despite contraindications pose a challenge in Fuchs’ dystrophy treatment.
Avoiding Posterior Capsule Rupture
Imaging may help, but surgical technique is key for managing posterior polar cataracts.