Hyperopia innovations
Adding donor stroma is new frontier for hyperopia, presbyopia, keratoconus treatment

Howard Larkin
Published: Monday, April 1, 2019
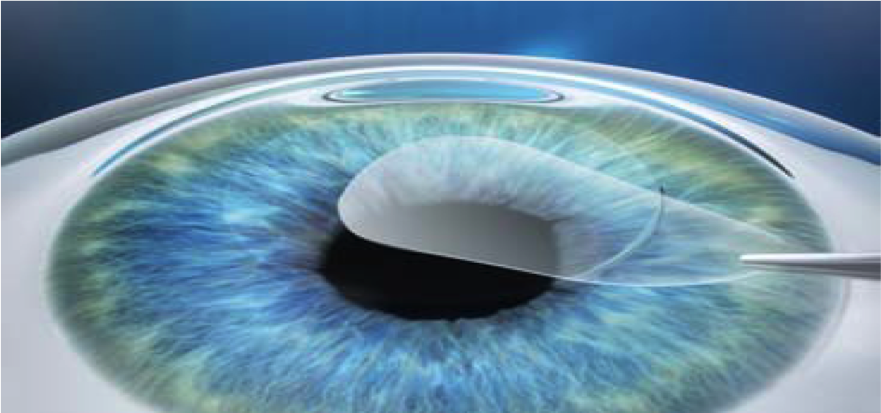 Extraction of SMILE lenticule from a myopic eye, which can be banked and later implanted in a hyperopic eye[/caption]
In 1949, José I Barraquer MD, the father of modern refractive surgery, formulated a simple, yet profound, law: if tissue subtraction from the centre of the cornea corrects myopia, then equal amounts of tissue addition should correct hyperopia of a similar magnitude.
Extraction of SMILE lenticule from a myopic eye, which can be banked and later implanted in a hyperopic eye[/caption]
In 1949, José I Barraquer MD, the father of modern refractive surgery, formulated a simple, yet profound, law: if tissue subtraction from the centre of the cornea corrects myopia, then equal amounts of tissue addition should correct hyperopia of a similar magnitude.
 Ronald R Krueger MD
Ronald R Krueger MD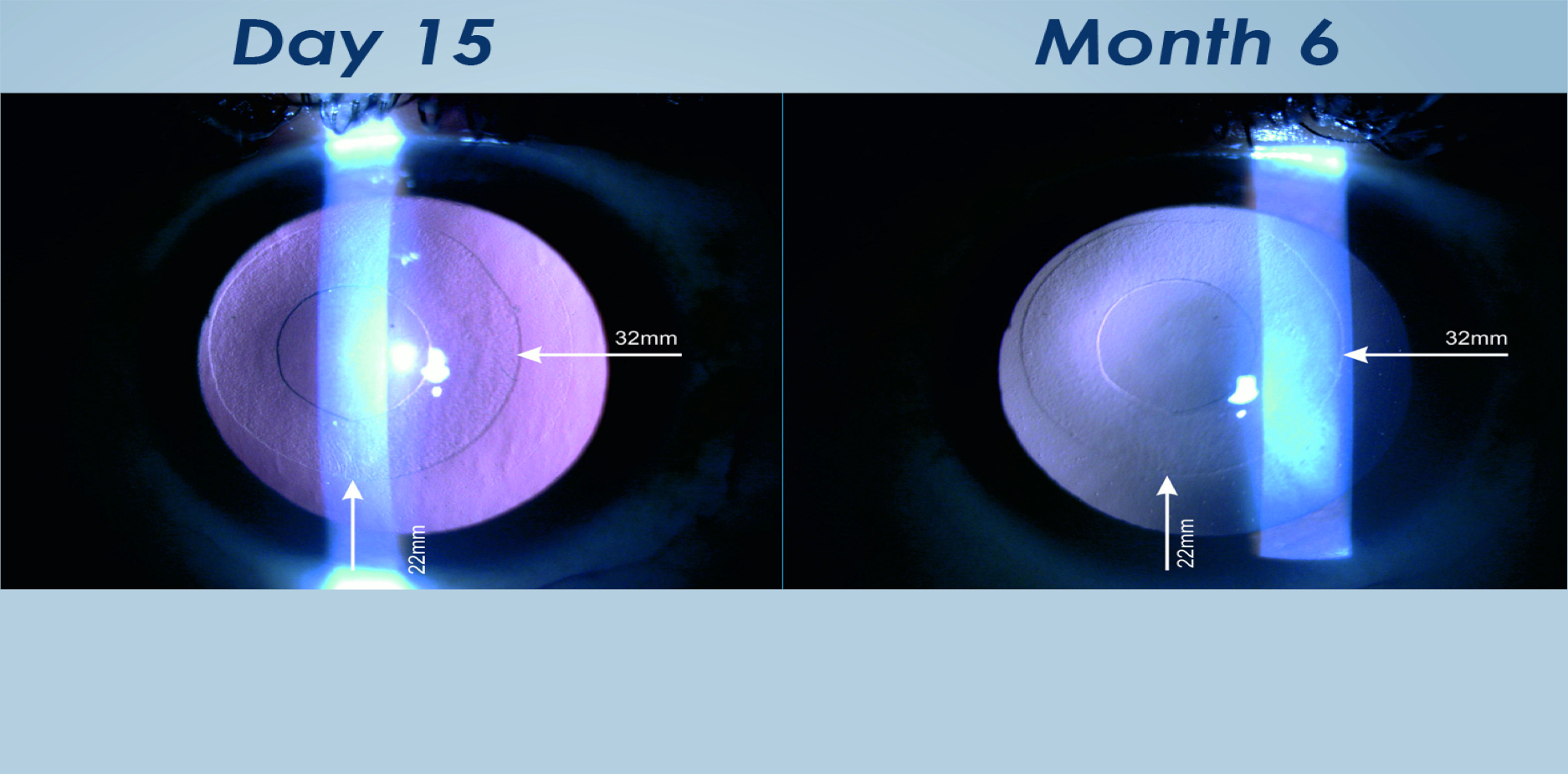 Slit lamp photo of a modified SMILE lenticule (annular) implanted into a central keratoconic eye, and viewed by retroillumination. (Courtesy of Sri Ganesh, Bangalore, India)[/caption]
In a yet unpublished Turkish study of 17 presbyopic eyes and 28 hyperopic eyes, implanting shaped, stromal tissue from a commercial source resulted in a mean central power increase of +2.7D for the correction of presbyopia and a mean uniform power increase of +6.0D for the correction of moderate to high hyperopia (personal communication Aylin Kilic MD and Michael Mrochen PhD). The commercial sources may cut many lenticules from a single donor and sterilise, process, package and store them at room temperature, Dr Krueger said. The surgeon can later open the packaging and shape them with a compact industrial excimer laser as needed.
LIKE – A NEW TECHNIQUE
Dr Krueger and others are beginning clinical investigation of a technique popularised by Dr Theo Seiler, called LIKE (lenticular implantation keratoplasty). This involves shaping donor corneal tissue with Bowman’s layer using a lenticule cavity unit, which defines the precise shape profile and power. The implanted lenticule power is targeted to be greater, and placed under the large LASIK flap of moderate-to-high hyperopia eyes, making it possible to later lift the flap for a myopic or customised ablation enhancement. In the first 12 eyes treated for up to +8.5D in Europe and India, five have so far received a laser ablation one-to-three months after implantation, and one required a replacement implant.
Of the first nine, no eye lost more than one line and three gained two lines at six months. Four had slight, temporary lenticular haze, less than typically seen with LASIK, Dr Krueger said. LIKE-shaped lenticules are also being shaped for treating keratoconus by placing the lenticule in a corneal stromal pocket.
“High hyperopia, presbyopia and keratoconus are just a few of the errors that will implement this technology in the future. Refractive eye-banking will be the emerging, new market and partnership that brings this technology to our field,”
Dr Krueger concluded.
Slit lamp photo of a modified SMILE lenticule (annular) implanted into a central keratoconic eye, and viewed by retroillumination. (Courtesy of Sri Ganesh, Bangalore, India)[/caption]
In a yet unpublished Turkish study of 17 presbyopic eyes and 28 hyperopic eyes, implanting shaped, stromal tissue from a commercial source resulted in a mean central power increase of +2.7D for the correction of presbyopia and a mean uniform power increase of +6.0D for the correction of moderate to high hyperopia (personal communication Aylin Kilic MD and Michael Mrochen PhD). The commercial sources may cut many lenticules from a single donor and sterilise, process, package and store them at room temperature, Dr Krueger said. The surgeon can later open the packaging and shape them with a compact industrial excimer laser as needed.
LIKE – A NEW TECHNIQUE
Dr Krueger and others are beginning clinical investigation of a technique popularised by Dr Theo Seiler, called LIKE (lenticular implantation keratoplasty). This involves shaping donor corneal tissue with Bowman’s layer using a lenticule cavity unit, which defines the precise shape profile and power. The implanted lenticule power is targeted to be greater, and placed under the large LASIK flap of moderate-to-high hyperopia eyes, making it possible to later lift the flap for a myopic or customised ablation enhancement. In the first 12 eyes treated for up to +8.5D in Europe and India, five have so far received a laser ablation one-to-three months after implantation, and one required a replacement implant.
Of the first nine, no eye lost more than one line and three gained two lines at six months. Four had slight, temporary lenticular haze, less than typically seen with LASIK, Dr Krueger said. LIKE-shaped lenticules are also being shaped for treating keratoconus by placing the lenticule in a corneal stromal pocket.
“High hyperopia, presbyopia and keratoconus are just a few of the errors that will implement this technology in the future. Refractive eye-banking will be the emerging, new market and partnership that brings this technology to our field,”
Dr Krueger concluded.
Tags: lenticular implantation keratoplasty (LIKE), SMILE
Latest Articles
Making Female Leadership More than a Moment
A remarkable global confluence of women in key positions.
ESCRS Talks Technology at AAO
Europe adopts technological advances, US still waiting for lenses and lasers.
Sorting Out Simultaneous Vision IOLs
The ESCRS Eye Journal Club discuss a new landmark paper on IOL classification and the need for harmonisation of terminology for presbyopic IOLs.
Big Advantages to Small-Aperture IOLs
Small-aperture IOLs offer superior image quality with increased range of focus.
Prioritising Self-Care
Benefits of maintaining physical, emotional, and mental health extend beyond the personal sphere.
Valuing Clinical Trial Design
How inclusivity and diversity can enhance scientific accuracy in research.
Knowing Iris Repair: Using Iridodiathermy in Iris Surgery
Prepare for decentred pupils and uneven irides in multiple situations.
Neuroprotectant Treatment for MacTel Type 2
Intravitreal implant releasing ciliary neurotrophic factor found safe and effective in pivotal trials.