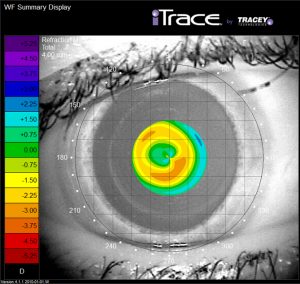
A major improvement in near vision is observed for
small pupils (ideal for 3.5 mm). The near “add”
effect of the Presbia Flexivue Microlens decreases for
large pupils (ideal for 6mm – corresponding to far vision)
The jury is still out on the safety and efficacy of current corneal inlays in the longer term, Ioannis Pallikaris MD, PhD, told a session of the 23rd ESCRS Winter Meeting in Athens.
“A variety of surgical options for presbyopia are now available, some are invasive and difficult or impossible to reverse. Corneal inlays, developed in the last decade, are designed to overcome those difficulties,” said Dr Pallikaris, University of Crete, Heraklion, Crete, Greece.
The corneal inlays are designed for implantation in the non-dominant eye in a pocket in the corneal stroma. The devices have employed a variety of optical approaches, generally aiming for a modified monovision with some degree of multifocality or extended depth of field. Several such devices have come and gone over the years, generally being withdrawn from the market because of biocompatibility issues.
Over the past five years, the USFDA has approved two new inlays, the KAMRA (Acufocus) small-aperture inlay in 2015 and the Raindrop – formerly produced by the now defunct company ReVision in 2016. Both inlays showed good initial results but in October 2018 the Raindrop was withdrawn from market after post-marketing surveillance revealed a 43% rate of corneal haze and a 23.3% explantation rate.
AND THEN THERE WERE TWO
That leaves only the KAMRA corneal inlay and the Presbia Flexivue Microlens. The USFDA clinical trial with the Flexivue lens has been completed and is expected to receive FDA approval some time in 2019, Dr Pallikaris said.
The KAMRA corneal inlay is designed to improve near vision while maintaining distance vision using the pinhole lens concept. The inlay has a diameter of 2.38mm, a thickness of 5.0 microns and is flexible enough to bend to different curvatures without buckling. It is opaque except for a 1.6mm aperture in the centre. It is implanted only in the non-dominant eye.
Through-focus visual acuity testing in eyes implanted with the devices show that there is considerable enhancement of depth of field compared to preoperative values, with about 2D range around the best focus when measured monocularly.
Eyes with the KAMRA inlay need to be near emmetropia preoperatively to achieve the best visual outcomes. Around 90% of eyes with manifest refraction spherical equivalent from -5D to -0.75D achieve 20/20 or better and J3, Dr Pallikaris reported.
The disadvantage of the KAMRA inlay’s small aperture is that less light contributes to the retinal image in one eye, which makes vision more difficult under mesopic or scotopic conditions.
Furthermore, reduced retinal illuminance in one eye can also causes a delay in that eye's transmission of the signal to the brain. That can result in a distortion in spatial perception known as the Pulfrich effect.
PULFRICH EFFECT
The Pulfrich effect is best known for the way it distorts the apparent path of a swinging pendulum, which will appear to follow an elliptical path as the small pupil sees the object where it was, not where it is.
Another potential problem with the KAMRA inlay is a postoperative hyperopisation that occurs in eyes with the device. For example, the Blue Mountains Eye Study showed that eyes with the implant had a hyperopic change equivalent to +0.4D over five years. Other postoperative issues reported for the KAMRA include blurred vision, diminished contrast sensitivity, diplopia, glare and halos.
The Presbia Flexivue Microlens is made of hydrophilic acrylic material and has a thickness of 0.015mm and a diameter of 3.2mm. The inlay has a higher refractive index than the corneal stroma. It is designed to provide a near add in the centre of the pupil so that the sharpest near image occurs in indoor lighting conditions.
In a study of eyes with the Microlens implant and up to five years of follow-up, the mean uncorrected near VA improved to J1 in 91.3% eyes of eyes and all eyes had an improvement of at least four lines of near vision.
Ioannis Pallikaris: pallikar@med.uoc.gr

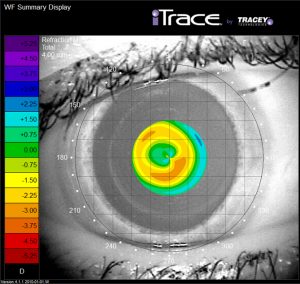 A major improvement in near vision is observed for
small pupils (ideal for 3.5 mm). The near “add”
effect of the Presbia Flexivue Microlens decreases for
large pupils (ideal for 6mm – corresponding to far vision)
A major improvement in near vision is observed for
small pupils (ideal for 3.5 mm). The near “add”
effect of the Presbia Flexivue Microlens decreases for
large pupils (ideal for 6mm – corresponding to far vision)