CAIRS for keratoconus
Donor corneal ring segments may be safer, more flexible than synthetic implants

Howard Larkin
Published: Monday, April 1, 2019
 For keratoconus patients treated with intrastromal ring segments, with or without corneal cross-linking (CXL), implants cut from donor corneas may be safer, and can be used in a broader range of cases, than segments of synthetic materials, said Soosan Jacob MS, FRCS, DNB, of Dr Agarwal’s Group of Eye Hospitals and Eye Research Centre, Chennai, India.
Complication rates for synthetic intrastromal ring segments run up to 30% in some studies and include problems such as extrusion, migration, neovascularisation, corneal melt, corneal necrosis and infection, said Dr Jacob. “The cornea does not tolerate synthetic materials well. So, why not use an allogenic substance instead?”
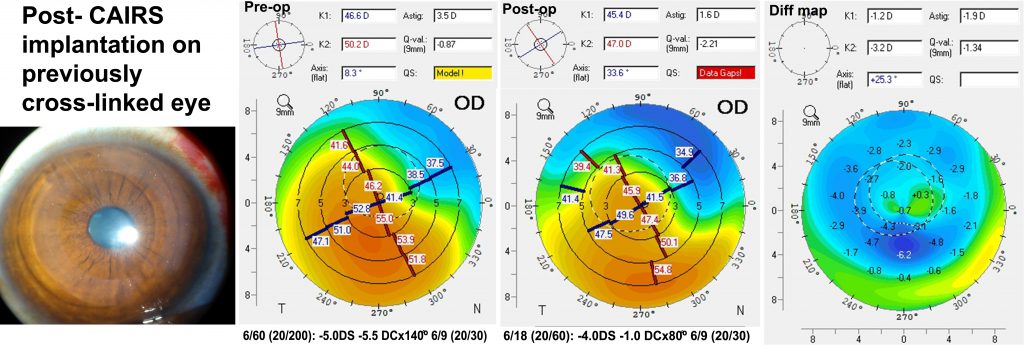
To reduce complications, Dr Jacob developed corneal allogenic intrastromal ring segments (CAIRS). As with synthetic ring segment surgery, CAIRS threads semi-circular inserts into channels cut by femtosecond lasers in the patient’s mid-peripheral stroma to reinforce and reshape the corneal surface, but the inserts themselves are cut from donor cornea tissue. CAIRS may be done with or without CXL depending on patient age, progression and whether previous CXL has been performed.
In more than 80 CAIRS patients treated through mid-February, Dr Jacob has seen excellent biocompatability, with follow-up ranging up to nearly three years. She believes this tolerance results from host keratocytes quickly repopulating the small amount of donor stroma, as happens in deep anterior lamellar keratoplasty (DALK) buttons, but quicker due to the much lower volume of tissue transplanted as well as the intrastromal placement. She treats patients with topical corticosteroids for six weeks after CAIRS, compared with four-to-six months after DALK, and mostly to control post-surgery inflammation rather than to prevent rejection.
MORE EFFECTIVE
High tolerance also makes allogenic ring segments more flexible than their synthetic counterparts, Dr Jacob said. Because they are less likely to extrude or cause corneal melt, allogenic implants may be inserted at 50% corneal depth or even more superficially, compared with 80% depth for synthetics. Placing the rings more superficially makes them more effective in reshaping the cornea, she noted. They can also be implanted in corneas thinner than the 450-500-micron limit for synthetic segments, Dr Jacob added.
“We can treat thinner corneas that are also steeper, which is a huge advantage. We have successfully treated many patients, from minimal cases to the most severe cases. If desired, allogenic segments may also be cut to different thicknesses, arc lengths and optical zone diameter as needed.”
Safety and efficacy has been quite good, Dr Jacob said. In a prospective study involving 24 eyes in 20 young patients undergoing CAIRS and accelerated CXL or accelerated CACXL (contact lens-assisted CXL – another technique described by Dr Jacob for thin corneas), all patients showed significant improvement in corrected and uncorrected visual acuity and corneal topography with no complications related to the implants.
Mean uncorrected distance visual acuity improved 2.79 lines ± 2.65, and mean corrected distance vision improved 1.29 ± 1.33 lines, and no loss of corrected or uncorrected VA in any eye. No progression was seen in any eye during follow-up, which averaged 11.58 months ranging from six-to-18 months (Jacob S et al. J Refract Surg 2018;34(5):296-303.).
As word spreads about the results she is achieving with CAIRS, many keratoconus patients from all over India are requesting treatment, Dr Jacob said. For those aged 30-to-40 or more with no signs of progression, CAIRS is typically done without CXL. “We are also offering it to our patients who have previously had cross-linking who want to improve their vision.”
In one case, a patient who had similar keratoconus in both eyes had CAIRS in one and CXL in both. The patient came back a year later for CAIRS in the other. Another patient with previous CXL had CAIRS in one eye and was so impressed he immediately asked for it in the other eye, Dr Jacob said.
Surgeons across India, the Middle East and the US are contacting her for adopting CAIRS. The procedure is easy to perform using a pull-through technique, Dr Jacob said. Next steps include femtosecond laser-cut donor segments, modified segments and storage development, she added.
Soosan Jacob: dr_soosanj@hotmail.com
For keratoconus patients treated with intrastromal ring segments, with or without corneal cross-linking (CXL), implants cut from donor corneas may be safer, and can be used in a broader range of cases, than segments of synthetic materials, said Soosan Jacob MS, FRCS, DNB, of Dr Agarwal’s Group of Eye Hospitals and Eye Research Centre, Chennai, India.
Complication rates for synthetic intrastromal ring segments run up to 30% in some studies and include problems such as extrusion, migration, neovascularisation, corneal melt, corneal necrosis and infection, said Dr Jacob. “The cornea does not tolerate synthetic materials well. So, why not use an allogenic substance instead?”
To reduce complications, Dr Jacob developed corneal allogenic intrastromal ring segments (CAIRS). As with synthetic ring segment surgery, CAIRS threads semi-circular inserts into channels cut by femtosecond lasers in the patient’s mid-peripheral stroma to reinforce and reshape the corneal surface, but the inserts themselves are cut from donor cornea tissue. CAIRS may be done with or without CXL depending on patient age, progression and whether previous CXL has been performed.
In more than 80 CAIRS patients treated through mid-February, Dr Jacob has seen excellent biocompatability, with follow-up ranging up to nearly three years. She believes this tolerance results from host keratocytes quickly repopulating the small amount of donor stroma, as happens in deep anterior lamellar keratoplasty (DALK) buttons, but quicker due to the much lower volume of tissue transplanted as well as the intrastromal placement. She treats patients with topical corticosteroids for six weeks after CAIRS, compared with four-to-six months after DALK, and mostly to control post-surgery inflammation rather than to prevent rejection.
MORE EFFECTIVE
High tolerance also makes allogenic ring segments more flexible than their synthetic counterparts, Dr Jacob said. Because they are less likely to extrude or cause corneal melt, allogenic implants may be inserted at 50% corneal depth or even more superficially, compared with 80% depth for synthetics. Placing the rings more superficially makes them more effective in reshaping the cornea, she noted. They can also be implanted in corneas thinner than the 450-500-micron limit for synthetic segments, Dr Jacob added.
“We can treat thinner corneas that are also steeper, which is a huge advantage. We have successfully treated many patients, from minimal cases to the most severe cases. If desired, allogenic segments may also be cut to different thicknesses, arc lengths and optical zone diameter as needed.”
Safety and efficacy has been quite good, Dr Jacob said. In a prospective study involving 24 eyes in 20 young patients undergoing CAIRS and accelerated CXL or accelerated CACXL (contact lens-assisted CXL – another technique described by Dr Jacob for thin corneas), all patients showed significant improvement in corrected and uncorrected visual acuity and corneal topography with no complications related to the implants.
Mean uncorrected distance visual acuity improved 2.79 lines ± 2.65, and mean corrected distance vision improved 1.29 ± 1.33 lines, and no loss of corrected or uncorrected VA in any eye. No progression was seen in any eye during follow-up, which averaged 11.58 months ranging from six-to-18 months (Jacob S et al. J Refract Surg 2018;34(5):296-303.).
As word spreads about the results she is achieving with CAIRS, many keratoconus patients from all over India are requesting treatment, Dr Jacob said. For those aged 30-to-40 or more with no signs of progression, CAIRS is typically done without CXL. “We are also offering it to our patients who have previously had cross-linking who want to improve their vision.”
In one case, a patient who had similar keratoconus in both eyes had CAIRS in one and CXL in both. The patient came back a year later for CAIRS in the other. Another patient with previous CXL had CAIRS in one eye and was so impressed he immediately asked for it in the other eye, Dr Jacob said.
Surgeons across India, the Middle East and the US are contacting her for adopting CAIRS. The procedure is easy to perform using a pull-through technique, Dr Jacob said. Next steps include femtosecond laser-cut donor segments, modified segments and storage development, she added.
Soosan Jacob: dr_soosanj@hotmail.com