Everything You Always Wanted To Know About...Pinhole Optics

Soosan Jacob
Published: Monday, May 1, 2023
“ The advantages of PPP are the ability to size and centre the pupillary aperture more accurately as well as cost efficiency. “
By Dr Soosan Jacob MS, FRCS, DNB
Ophthalmologists have used pinholes for more than 100 years to aid in the diagnosis and treatment of visual problems, such as pinhole occluders for testing visual potential and pinhole glasses. The small aperture allows light from a single source and direction to fall upon the retina while at the same time also removing scattering, thereby allowing an individual with refractive error to see clearly. This results in an extended depth of focus as well as clearer vision by reduction of both lower and higher order aberrations.
Pinhole IOLs
The IC8 intraocular lens (Acufocus) is a 5-micron thick annular ring composed of polyvinylidene fluoride and carbon nanoparticles embedded in a single-piece hydrophobic acrylic IOL. The inner and outer diameters are 1.36 and 3.23 mm respectively. It is implanted in the non-dominant eye to provide increased depth of focus and 3.0 D functional range of presbyopic correction. It can also correct astigmatism up to 1.5 D and in some cases, even up to 2.5 D; combine with mild residual refractive error of -0.75 D to increase presbyopic correction further; and be used in patients with previous radial keratotomy or LASIK where other presbyopic IOLs may result in sub-optimal correction.
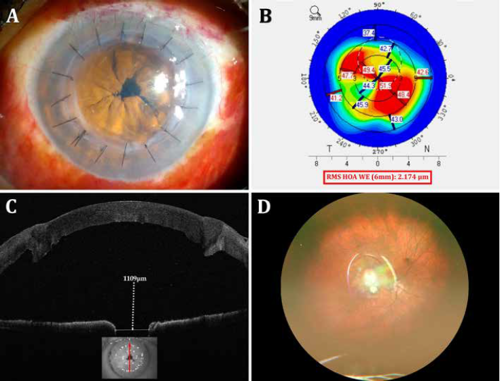
The XtraFocus Pinhole intraocular lens implant (Morcher) was first introduced in 2014 by Trindade (et al.) and received the CE mark in 2016. This foldable hydrophobic acrylic 14.0 mm diameter sulcus IOL with 6.0 mm optic is opaque and black with a 1.3 mm central clear aperture without any refractive power. It is used mainly for treating irregular astigmatism secondary to penetrating keratoplasty, radial keratotomy, and keratoconus.
Its pinhole effect neutralizes the effect of corneal aberrations. The black pigment of this sulcus-placed IOL allows infrared rays to pass through, enabling fundus examination and providing view of the retro-IOL structures, such as the in-the-bag IOL placed behind it. Implanted through a small incision, the XtraFocus may even be implanted in the bag, together with primary IOL implantation, the concave-convex design preventing primary IOL touch. Previous use includes treating irregular astigmatism in complex eyes.
Both the IC8 and XtraFocus IOLs may produce photic phenomena in patients with large mesopic pupil size greater than 6.0 mm, where light may enter around the external diameter of the opaque annulus or the optic.
Pinhole Pupilloplasty (PPP)
First described by Professor Amar Agarwal, pinhole pupilloplasty (PPP) reduces pupil size surgically and can be done in pseudophakic eyes or in combination with cataract surgery and IOL implantation. Surgeons preoperatively test a range of pupil sizes to determine the ideal pupil size for the patient, which then becomes the surgical aim. They centre the PPP on the first Purkinje reflex marked preoperatively on the slit lamp. Though possible to complete using the surgeon’s choice of pupilloplasty technique, it is commonly done using the single-pass four-throw pupilloplasty.
Advantages of PPP are the ability to size and centre the pupillary aperture more accurately as well as cost efficiency. The pinhole pupil can be cantered under the first Purkinje reflex even in patients with large chord mu values, unlike pinhole IOLs which centre automatically in the bag or sulcus. Fundus visualisation is possible since the dilator muscles still act to enlarge the parts of the pupil that are not tied down. In addition, newer wide-angle retinal imaging systems can capture fundus images even through undilated small pupils. However, it is not possible in phakic eyes and in eyes where iris tissue is missing over large areas, such as in post-traumatic or post-surgical iris loss.
Corneal inlays
The Kamra intracorneal inlay (CorneaGen) has been implanted in more than 20,000 eyes, although the manufacturer discontinued the product in the US in February 2022. It is used for presbyopia correction in the non-dominant eye in both phakic and pseudophakic patients. It is a 3.8 mm diameter, 6 microns thick opaque corneal inlay with microperforations and a 1.6 mm central opening—implanted in a femtosecond laser-dissected pocket within the corneal stroma. Haze and refractive shift were seen in a small percentage of patients, though combining with laser vision correction to obtain a slight myopic shift helped achieve better results.
Miotic drops
As another option, miotic drops induce a pinhole effect through the parasympathetic pathway. Recently approved by the US FDA for treating presbyopia, topical 1.25% pilocarpine (Vuity, Allergan) can be used uniocularly for monovision or in both eyes. They may cause headaches and dim vision at night. Long-term safety and efficacy are not known, but long-term miotic use has previously been associated with chronic inflammation and retinal detachment.
Other investigated miotic agents include brimonidine, phentolamine, carbachol, aceclidine, AGN-241622, CSF-1, and drug combinations. The need for daily dosing, issues with tolerance, and inability to address refractive error and cataract are disadvantages.
Pinhole aperture optics
Mostly used monocularly, pinhole optics find use in certain situations, such as bilateral radial keratotomy or bilateral corneal grafts with high irregular astigmatism, where it may be used in both eyes. Despite the possibility that small aperture optics could lead to difficulty in low light conditions, there have been contrasting reports. Trindade (et al.) had only one of 21 patients complain of reduced acuity. Perceived brightness through small apertures showed 1.25 to 1.5 times more than expected from the aperture size because of the Stiles-Crawford effect, binocular effect, and other unknown effects.
In monocular surgeries, binocularity also helps increase perceived brightness. Binocularity has shown to provide better contrast sensitivity than multifocal IOLs—and though some drop shows at certain lighting conditions or spatial frequencies, in unilateral surgeries, there is very little change in binocular contrast sensitivity. Additionally, making the pupil too small may result in image degradation from diffraction, so surgeons should avoid extremely small pinholes, especially when attempting to treat presbyopia.
Diagnostic tests before surgery include uncorrected and best spectacle- corrected visual acuity followed by pinhole testing on the spectacle refraction, visual acuity with rigid contact lens, topography, and aberrometry. Other tests, such as dominance and macular OCT, may be decided based on specific patient characteristics and needs.
Pinhole optics should be avoided in patients with scars in the cornea. Some of the devices and procedures can however be tried in patients with iris defects and those unhappy with multifocal IOLs. The pinhole can get rid of the symptoms in patients with night vision disturbances, such as halos from multifocal IOLs, while still providing sharp vision and an extended depth of focus.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India, and can be reached at dr_soosanj@hotmail.com.