Cataract, Refractive, Cataract and Refractive Articles, Issue Cover
Which Farsighted Fix?
Evolving technologies opening new doors to best treatments.
Cheryl Guttman Krader
Published: Friday, November 1, 2024
Lenticule extraction with the VISUMAX 800 femtosecond laser (SMILE pro) is now available in CE markets as an alternative to LASIK for treating hyperopia. Results from the multicentre study that supported regulatory approval of the femtosecond laser-based procedure demonstrate its effectiveness and safety, but also indicate it may offer better refractive stability compared to LASIK, according to Glenn I Carp MD.1
Lenticule extraction in the multicentre study was performed using the VisuMax laser.1 It included 374 eyes with up to +6.00 D sphere and up to -5.00 D cylinder.
“It was amazing that at 12 months, 81% of eyes were within 0.50 D of targeted refraction and 93% were within 1.00 D,” Dr Carp said. “There was less regression than after LASIK, and of course, good safety.”
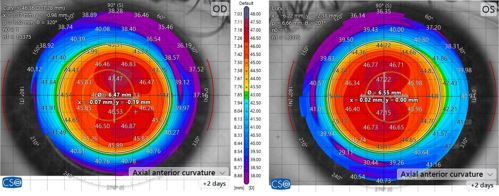
He proposed the study achieved a larger effective optical zone (OZ) post-SMILE versus post-LASIK, which may explain the difference in regression seen postoperatively. Reviewing data from eyes treated with SMILE using a 6.3 mm OZ and 2.0 mm transition zone, Dr Carp emphasised the achieved topographically-measured OZ was consistently larger after SMILE than after LASIK using either a 6.5 mm OZ or a 7.0 mm OZ in LASIK.2 (see Figure 3)
“The difference is because the cornea, biomechanically, behaves very differently after the two procedures,” he said.
“The most likely reason for the effective larger zone is that there is less peripheral expansion of fibres after SMILE compared to LASIK and, therefore, less shortening of the OZ. This also probably explains why the refraction is more stable after SMILE—less regression, suggesting SMILE might also provide better optical quality.”
Optimising outcomes after LASIK
Discussing hyperopic LASIK, Dr Carp noted research conducted at the London Vision Clinic, UK, provides guidance on treating high hyperopia/hyperopic astigmatism.3 He focused on the proper technique for ablation centration and deciding on the correction limit for a given eye.
“LASIK for higher levels of hyperopia can be done with reliable safety by centring the ablation on the visual axis and respecting epithelial thickness,” he advised.
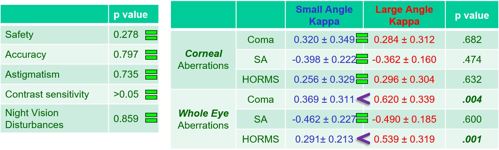
Evidence supporting centring the ablation on the visual axis (i.e., the coaxially sighted corneal light reflex, CSCLR) rather than the Benham of the entrance pupil comes from findings of a retrospective study comparing outcomes of hyperopic LASIK in eyes with a small (≤0.25 mm) versus large angle kappa (≥0.55 mm).4,2 All treatments centred on the CSCLR, and the postoperative results showed no differences between groups in safety, accuracy, induced astigmatism, contrast sensitivity, night vision disturbances, or corneal aberrations.
“Patients with a small angle kappa were effectively treated with pupil-based centration, and if it is correct that the treatment should be pupil-centred, the eyes with a large angle kappa would have had a decentred ablation. [These eyes] should have had poorer vision with higher levels of corneal aberrations. The fact that the outcomes were similar supports the visual axis centration hypothesis,” said Dr Carp, adding other published literature shows consensus on the topic. (see Figure 2)
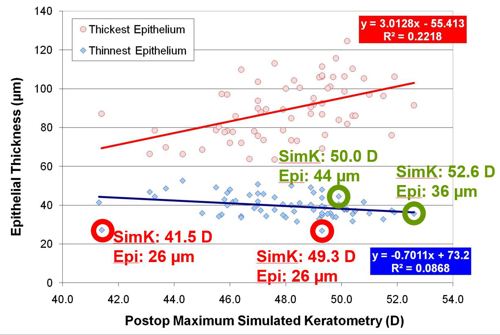
Addressing limits for LASIK treatment of hyperopia/hyperopic astigmatism, Dr Carp said the amount of correction that can be safely done is determined by considering post-treatment epithelial thickness rather than keratometry.
“Most surgeons will tell you that when performing hyperopic LASIK, you should not steepen the cornea above 49.00 D because excessive steepening can lead to epithelial breakdown (apical syndrome),” he said. “What is more important for understanding epithelial breakdown is to look at the rate of change of curvature of the stromal surface.”
Dr Carp’s research at the London Vision Clinic shows that overall, the central epithelium progressively thins and the peripheral cornea progressively thickens the higher the attempted correction and postoperative keratometry value.3 However, he noted outliers to this pattern, presenting cases of hyperopic LASIK-treated eyes with a thin central epithelium and flat cornea and others with a thick central epithelium despite a steep cornea (>49.00 D).
“Some flat corneas will already have excessive central epithelial thinning, but some steep corneas can be steepened further if the epithelial thickness is sufficient,” Dr Carp said. (see Figure 1)
The key for reducing the risk of apical syndrome is to respect the 26-micron limit for central epithelial thickness integrity, meaning that treatment leading to a central epithelial thickness of less than 30 microns should be avoided. The epithelial thickness studies in hyperopic LASIK show an average of 2 microns of thinning per dioptre treated. These studies were conducted with VHF digital ultrasound epithelial measurements, showing these limits may differ for OCT-based epithelial measurements. Applying this principle to clinical practice supports a two-stage approach to LASIK for high hyperopia where an initial conservative correction is done epithelial thickness monitoring guides the decision about an enhancement.
Dr Carp observed another study found this protocol resulted in safe, effective, and stable outcomes in a large cohort of eyes with +4.00 D to +9.00 D maximum hyperopia.4 Primary treatment was limited up to +6.50 D hyperopia. Epithelial thickness was measured at one year using very high-frequency digital ultrasound to evaluate the potential for a second treatment. In this study, 20% of eyes were treated as a planned two-stage procedure.
“The results were amazing for two years. The postoperative SEQ was within 0.50 D of attempted in 67% of eyes and within 1.00 D in 89%. Safety was excellent as well, and these results compare very well with other studies using other lasers,” Dr Carp said. “Providing clinicians treatment planning considerations with respect to centration on the visual axis (coaxially sighted corneal reflex) and the limits of epithelial remodelling, they can safely treat patients in the high hyperopic group. We recommend a limit of no greater than +6.50 D at the primary treatment. In such cases, if anterior chamber depth and the anterior chamber angle permit, then an ICL can also be considered.”
Dr Carp spoke at the 2024 ESCRS Congress during the ESCRS Refractive Surgery IME symposium, “Maximizing visual quality through enhanced precision and safety.”
Glenn I Carp MD is an ophthalmic surgeon at London Vision Clinic, London, UK. glenn@londonvisionclinic.com
1. Reinstein DZ, Sekundo W, Archer TJ, et al. “SMILE for Hyperopia with and Without Astigmatism: Results of a Prospective Multicenter 12-Month Study,” J Refract Surg, 2022; 38(12): 760–769.
2. Reinstein DZ, Pradhan KR, Carp GI, Archer TJ, Gobbe M, Sekundo W, Khan R, Dhungana P. “Small Incision Lenticule Extraction (SMILE) for Hyperopia: Optical Zone Diameter and Spherical Aberration Induction,” J Refract Surg, 2017 Jun 1; 33(6): 370–376.
3. Reinstein DZ, Carp GI, Archer TJ, et al. “LASIK for the Correction of High Hyperopic Astigmatism with Epithelial Thickness Monitoring,” J Refract Surg, 2017; 33(5): 314–321.
4. Reinstein DZ, Gobbe M, Archer TJ. “Coaxially sighted corneal light reflex versus entrance pupil center centration of moderate to high hyperopic corneal ablations in eyes with small and large angle kappa,” J Refract Surg, 2013; 29(8): 518–525.