Santen Vision 2030
MicroShunt pending FDA approval exemplifies new focus on unmet patient need

Howard Larkin
Published: Thursday, October 1, 2020
 Omar Sadruddin MD
Omar Sadruddin MD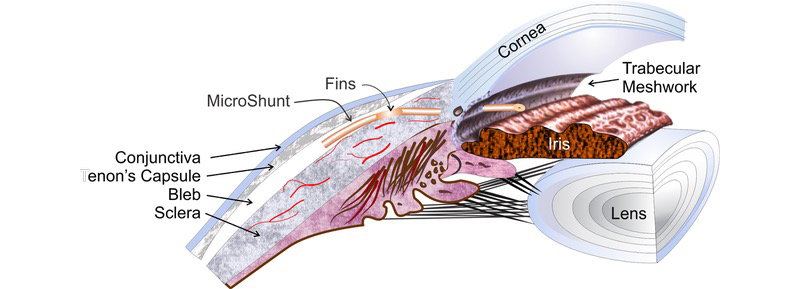 After marking the sclera 3mm from the limbus, a 1mm-deep scleral pocket is made using a triangular knife. A 25-gauge needle is introduced into the pocket and a scleral needle track is created into the AC. The MicroShunt is inserted through the pocket and track, bevel-up, into the AC. When correctly placed, the MicroShunt should bisect the angle without touching the endothelium or the iris. The fin is tucked in the scleral pocket. After flow is established, Tenon’s and conjunctiva are pulled up, avoiding tucking the distal end of the tube into Tenon’s capsule, and sutured watertight.
MicroShunt is designed for POAG patients whose IOP is not well controlled on maximum tolerated meds, Dr Sadruddin said. But if the ease of earlier intervention and long-term efficacy pan out, the definition of maximum meds may change from three or more to two – particularly given there is ample research suggesting that adding more meds don’t necessarily lower pressures significant for a long duration.
While implantable with or without cataract surgery, Dr Sadruddin sees glaucoma specialists as the primary target clinicians due to the need to manage the bleb. He sees MicroShunt as another tool in the armamentarium for customising treatment. “If you want an IOP <15mmHg for your patient, and the only remaining options are trab or tubes, MicroShunt may be a reasonable alternative.”
Santen offers a structured course for implanting the device that includes didactic material, virtual simulator and wet labs, as well as supervised procedures. Dr Sadruddin credits having a standardised technique to the users of the product and their willingness to share nuances and pearls of the procedure with new users. “By having created a community of MicroShunt users, we continuously focus on ways to optimise the technique and bring that education to current and future users of the MicroShunt.”
He acknowledged, however, that more long-term studies need to be done to validate the device performance and clinical results. These may include remote sensor studies to monitor IOP 24 hours a day.
“We have made strategic investments in companies looking at sensors. It’s a way to provide more feedback to surgeons to create better management plans, which allows to preserve as much of the patient’s vision as possible,” Dr Sadruddin said. It’s another way Santen is innovating in service of patients.
After marking the sclera 3mm from the limbus, a 1mm-deep scleral pocket is made using a triangular knife. A 25-gauge needle is introduced into the pocket and a scleral needle track is created into the AC. The MicroShunt is inserted through the pocket and track, bevel-up, into the AC. When correctly placed, the MicroShunt should bisect the angle without touching the endothelium or the iris. The fin is tucked in the scleral pocket. After flow is established, Tenon’s and conjunctiva are pulled up, avoiding tucking the distal end of the tube into Tenon’s capsule, and sutured watertight.
MicroShunt is designed for POAG patients whose IOP is not well controlled on maximum tolerated meds, Dr Sadruddin said. But if the ease of earlier intervention and long-term efficacy pan out, the definition of maximum meds may change from three or more to two – particularly given there is ample research suggesting that adding more meds don’t necessarily lower pressures significant for a long duration.
While implantable with or without cataract surgery, Dr Sadruddin sees glaucoma specialists as the primary target clinicians due to the need to manage the bleb. He sees MicroShunt as another tool in the armamentarium for customising treatment. “If you want an IOP <15mmHg for your patient, and the only remaining options are trab or tubes, MicroShunt may be a reasonable alternative.”
Santen offers a structured course for implanting the device that includes didactic material, virtual simulator and wet labs, as well as supervised procedures. Dr Sadruddin credits having a standardised technique to the users of the product and their willingness to share nuances and pearls of the procedure with new users. “By having created a community of MicroShunt users, we continuously focus on ways to optimise the technique and bring that education to current and future users of the MicroShunt.”
He acknowledged, however, that more long-term studies need to be done to validate the device performance and clinical results. These may include remote sensor studies to monitor IOP 24 hours a day.
“We have made strategic investments in companies looking at sensors. It’s a way to provide more feedback to surgeons to create better management plans, which allows to preserve as much of the patient’s vision as possible,” Dr Sadruddin said. It’s another way Santen is innovating in service of patients.