Cornea, Patient Journey
Patients Worth Fighting For
One clinician emphasises the value of treating cases involving some of the most catastrophic damage ever seen.

Andrew Sweeney
Published: Monday, November 3, 2025
“ Something that I’ve learned at this job, and with Patient K as well, is that the most hopeless eyes are the ones most worth fighting for. “
When Patient K took his first hit of cocaine, it likely didn’t cross his mind that his body would suffer serious damage. However, nobody—not even the most stringent of physicians—would have predicted it would cost him both of his eyes.
Patient K hails from the United Kingdom, a country in the midst of a cocaine epidemic, with lifetime use among adults rising from 5.1% in 2001 to 10.3% in 2023.1 Drug poisoning deaths are at an all-time high, but the popularity of the drug shows no sign of abating.
Most cocaine users will not likely be able to match Patient K’s record of drug abuse. He was a consistent user for more than 20 years, but over the last 5, he took a minimum of 2 grams per day—amounting to 730 grams per year—combined with daily tobacco usage of 20–30 cigarettes.
By the time he met Magdalena Niestrata MBChB, PhD, he already had a deviated septum, his left orbital wall had collapsed, and he had lost his right eye due to endogenous endophthalmitis—and this wasn’t even the most shocking damage she found.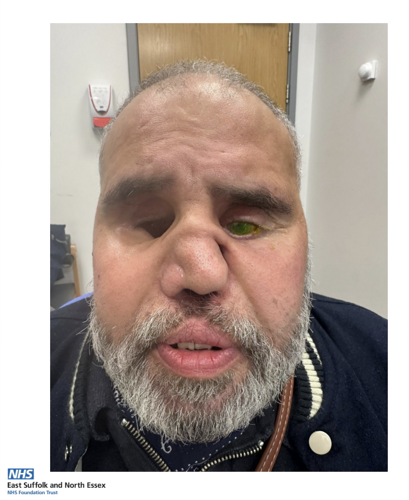
“Patient K effectively had no interior wall. So, when you looked through where his other eye used to be, you could see up to the other side of the skull,” said Dr Niestrata.
“The left eye had developed severe, chronic corneal melt with five perforations. The patient had visual acuity of 2/60, IOP was 5 mmHg, and inferior corneal melt equalled more than two-thirds stromal loss with iris-plugged perforation.”
When it rains, it pours
Unfortunately for Patient K, the damage to his body, so severe that he currently requires a prosthesis to talk and eat, wasn’t solely due to cocaine use. Not only had he developed vasculitis, but he’d been unlucky enough to develop a specific type of the autoimmune disease characterised by the presence of anti-neutrophil cytoplasmic antibodies (ANCAs).
In essence, the body was already attacking itself while also experiencing the effects of decades of cocaine abuse. According to Dr Niestrata, Patient K’s case was among the worst she’s ever seen.
“The damage was so severe. When we were putting lenses in the remaining eye, he kept losing the lenses, and it took us a while to figure out why,” she said. “We discovered that they were falling into his skull, as there was no soft tissue to support them.”
The extremity of Patient K’s case also extended to the surgeries Dr Niestrata had to perform. Over the course of nine months, she carried out the following procedures:
Three multilamellar amniotic-membrane overlays; two halo corneal grafts, one intrastromal inlay, one tectonic patch; two tectonic penetrating keratoplasties with multiple corneal gluing; one tectonic Descemet stripping with automated endothelial keratoplasty; two collagen cross-linking procedures; four staged tarsorrhaphies involving a Gundersen flap and tenon translocation; cataract surgery; vitrectomy; and multiple intravitreal injections for endophthalmitis.
All these procedures had to be performed with local anaesthetic only, as the damage to Patient K’s throat was severe enough to compromise his breathing. Multiple complications arose, too, including several corneal perforations, superimposed bacterial and fungal keratitis, and bacterial and fungal endophthalmitis.
A patient worth fighting for
Despite the remarkable challenges at play, these procedures initially worked. Patient K’s globe was successfully preserved, with sight restored to the degree that he could see hand movement and perceive light.
Dr Niestrata reported her case study highlighted that early aggressive immunosuppression, rapid surgical escalation, and persistent follow-up can rescue even a severely compromised, single-seeing eye. Unfortunately, there has since been unwelcome news.
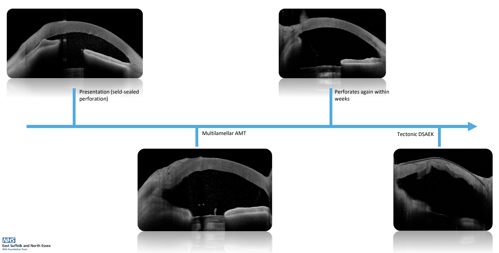
“During treatment for a second round of endophthalmitis, he received between four and five intravitreal injections. He developed a funnel retinal detachment, and the cornea began to melt completely,” Dr Niestrata said.
“He’s now completely blind; he is also experiencing symptoms of heart failure and some hallucinations as well. It’s obviously very disappointing as the cornea just kept melting. We really fought for it, but at least we were able to give him some sight for nearly another year.”
Even with this difficult-to-accept result, both Dr Niestrata and her patient maintain a positive attitude about the attempt to save his sight. Since undergoing his treatment, Patient K has become focused on being an advocate for greater awareness about cocaine toxicity and vasculitis, and Dr Niestrata believes this case study can provide valuable lessons to fellow clinicians.
“Something that I’ve learned at this job, and with Patient K as well, is that the most hopeless eyes are the ones most worth fighting for. He was fighting for light perception in just one eye; it really puts things into perspective,” Dr Niestrata said.
“We knew it was going to be difficult, and other clinics Patient K went to said the cornea would melt anyway, so they basically turned him away. We knew he was worth fighting for.”
Magdalena Niestrata PhD(Dist), MSc(Dist), MBChB(Hons), BSc(Hons), PGDip(Dist), FRCOphth, FEBO, FICO is a Corneal Fellow at the East Suffolk and North Essex Hospital Trust, Colchester, UK. magdalena.niestrata@doctors.org.uk
1. “The Rise of Cocaine Usage in the UK,” UK Addition Treatment Centres, 29 Apr 2025, https://www.ukat.co.uk/blog/substance-abuse/the-rise-of-cocaine-usage-in-the-uk/