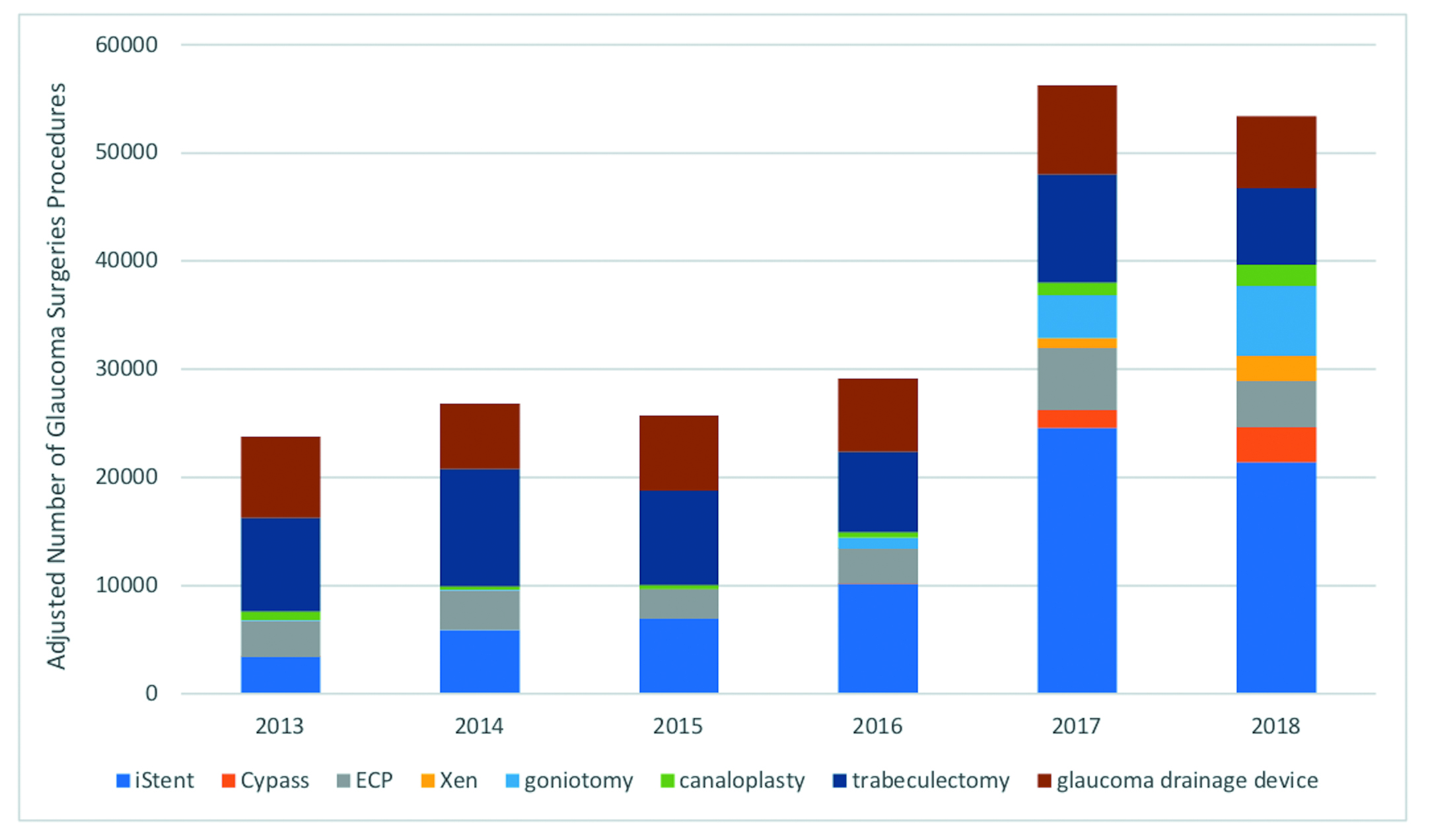
MIGS Jumps in USA
6-year study finds use doubles as standard glaucoma surgeries decline. Howard Larkin reports.

Howard Larkin
Published: Wednesday, June 30, 2021
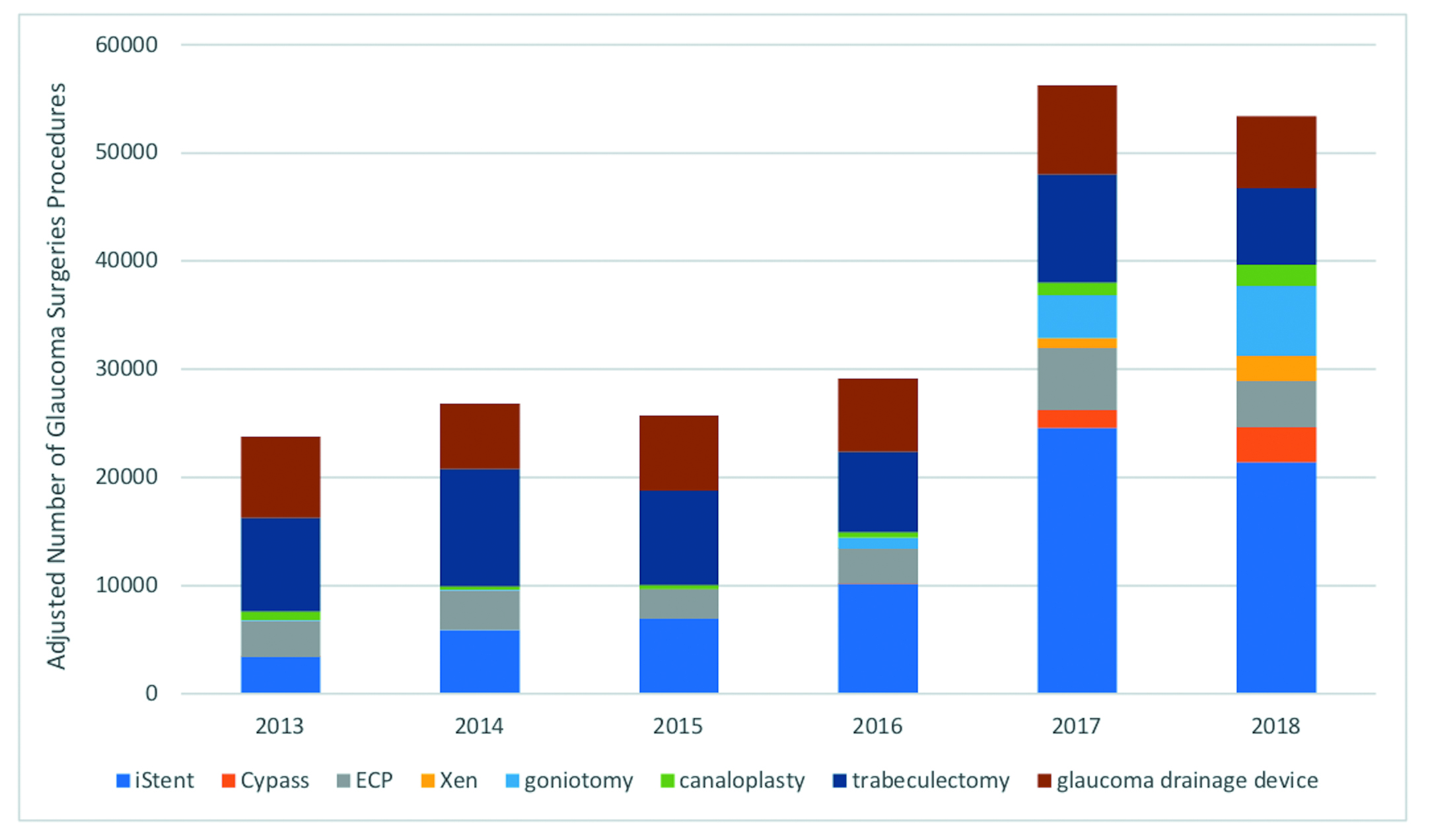
6-year study finds use doubles as standard glaucoma surgeries decline. Howard Larkin reports.

Published: Wednesday, June 30, 2021