Cataract, Refractive, IOL
Matching Premium IOLs to Visual Lifestyles
From monofocal to full-range solutions, each practice needs comprehensive understanding.

Cheryl Guttman Krader
Published: Wednesday, October 1, 2025
The growing arsenal of intraocular lens (IOL) options gives cataract surgeons more opportunities to meet their patients’ visual goals. However, greater choice also brings added responsibility, as surgeons must be knowledgeable about the optical principles and bench performance of several IOLs to recommend the best possible match for each patient’s visual lifestyle. Furthermore, optimizing the chance of success and patient satisfaction also requires that cataract surgeons implement what they have learned from their personal clinical experience and provide appropriate patient education to establish realistic expectations, says Andreas F Borkenstein MD.
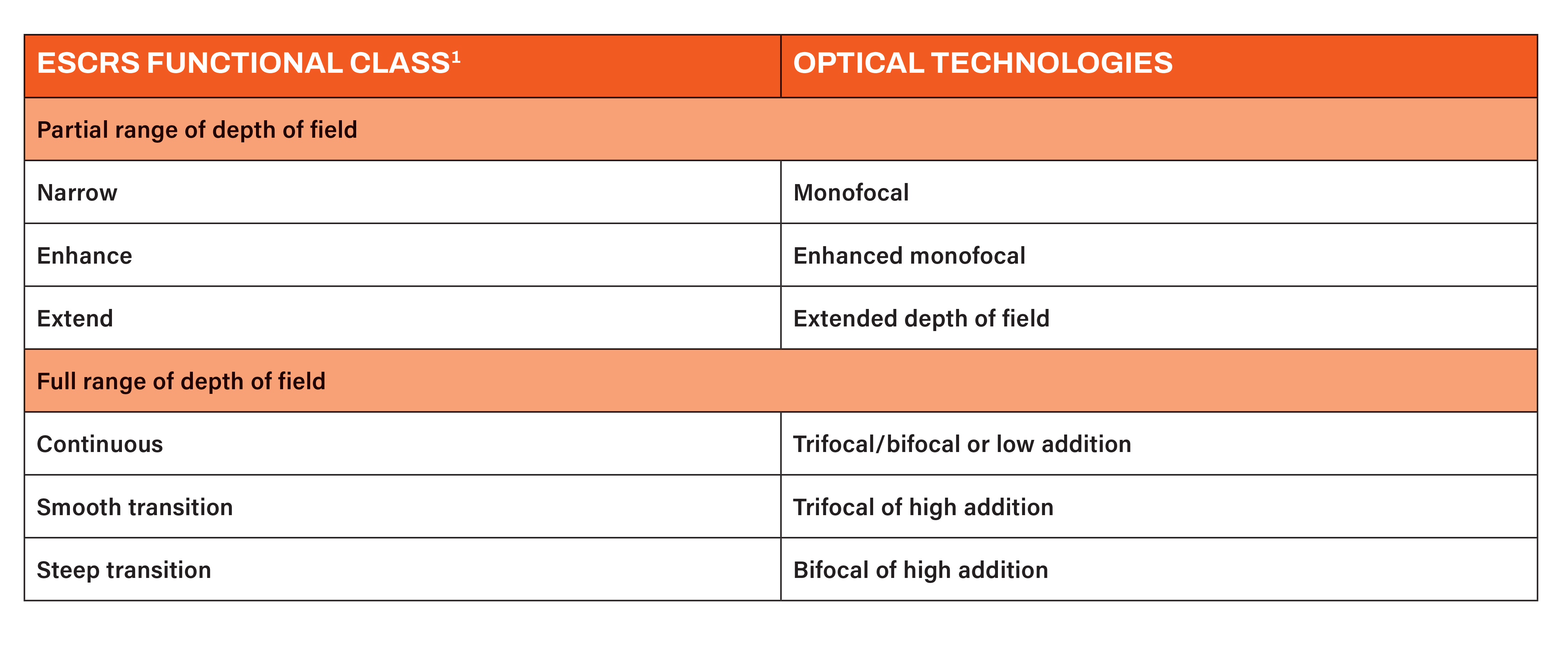
“An IOL classification system recently proposed by the European Society of Cataract and Refractive Surgeons (ESCRS) categorizes IOLs in a clinically relevant manner by differentiating them based on functional visual outcomes defined by defocus curve metrics rather than by optical design,”1 Dr Borkenstein said. “This classification system provides a valuable framework for understanding and implementing IOL technologies. However, surgeons must also be aware [of the] differences between the various categories with respect to patient adaptation and photic phenomena that must be discussed with patients and are not covered by the functional classification.”
Expanding on these issues, he explained that enhanced monofocal and extended depth of field (EDOF) IOLs, both of which the ESCRS system classifies as partial range of depth of field IOLs (see table), typically offer a smoother adaptation period and are associated with fewer photic disturbances compared to IOLs with a full range of depth of field.
“Nonetheless, proper IOL centration and proper informed consent can mitigate patient dissatisfaction because of these issues,” Dr Borkenstein said.
Preoperative and postoperative considerations
Preoperative consultation should involve a thorough assessment of the patient’s lifestyle, visual needs, and tolerance for potential side effects. Patients who spend significant time at intermediate distances (e.g., computer work) may benefit more from enhanced or extended range of field IOLs, while those desiring maximum spectacle independence, including for reading, may be candidates for full range of field IOLs. Alternatively, surgeons can implement a ‘mix and match’ approach combining different IOL types for binocular implantation or a monovision approach targeting a different refraction in each eye.
“These techniques can enhance the overall range. It is essential, however, to have a detailed discussion with the patient beforehand, covering the advantages and limitations in daily life, to understand [their] occupational and recreational needs and jointly define a clear target refraction,” Dr Borkenstein said.
“Additionally, digital simulation tools can help patients visualize their postoperative vision, improving satisfaction and consent quality. These tools enable patients to perceive differences in contrast sensitivity, depth of focus, and potential photic phenomena with different IOLs and can support informed decision-making, especially when considering more complex lens profiles like extended or full range of focus. For visually demanding patients, this individualized approach can also significantly improve satisfaction and reduce postoperative surprises.”
Integrating EDOF and full range of field IOLs into clinical practice also requires a structured workflow and the appropriate infrastructure. As essential diagnostic tools for surgical planning, Dr Borkenstein recommended optical coherence biometry for accurate axial length measurement, corneal topography for mapping astigmatism, and wavefront aberrometry to detect higher-order aberrations.
Postoperatively, the follow-up protocol should include early assessment of uncorrected visual acuity, lens centration, and patient-reported outcomes. Minor residual refractive errors may be addressed with glasses or laser touch-up procedures, while significant dissatisfaction should prompt re-evaluation of lens alignment or selection. However, the role of neuroadaptation should not be overlooked, Dr Borkenstein said.
“As the brain adjusts to simultaneous image processing from different focal zones, visual perception may evolve significantly over time—often within three to six months,” Dr Borkenstein said. “While many patients adapt naturally, others may benefit from targeted visual training or supportive counselling during the early postoperative phase. Addressing this process proactively can enhance outcomes and reduce the risk of dissatisfaction in the adaptation period.”
He also reminded his colleagues of the importance of comprehensive training for all medical staff interacting with patients, ensuring the entire team is well-versed in the optical characteristics and possible side effects of the available IOLs and effective counselling strategies related to these topics. Educational materials, such as brochures, model IOLs, and simulation software, can further enhance patient understanding and decision making.
“Creating a successful premium IOL practice is not just about offering a range of products. Understanding the optical principles behind various IOL designs is essential. This underscores the importance of experimental research and optical bench testing—efforts [to which] I am personally committed. For those without direct access to such investigations, studying peer-reviewed optical performance data is vital to building a sound foundation before clinical application and, ultimately, personal experience with each lens,” Dr Borkenstein said.
“Then, appropriate diagnostics, surgical precision, and patient engagement to deliver a personalized experience can help surgeons achieve their patients’ visual goals and satisfaction.”
Andreas F Borkenstein MD is a consultant ophthalmic surgeon at the Privatklinik der Kreuzschwestern and co-owner of Borkenstein & Borkenstein Research & Laboratory Gmbh, both in Graz, Austria. crustalith@gmx.at
1. Ribeiro F, Dick HB, Kohnen T, et al. J Cataract Refract Surg, 2024; 50(8): 794–798.