Cornea, Corneal Therapeutics
Knowing Iris Repair: Iris Cerclage
Part six in a series on iris repair.

Soosan Jacob
Published: Thursday, August 1, 2024
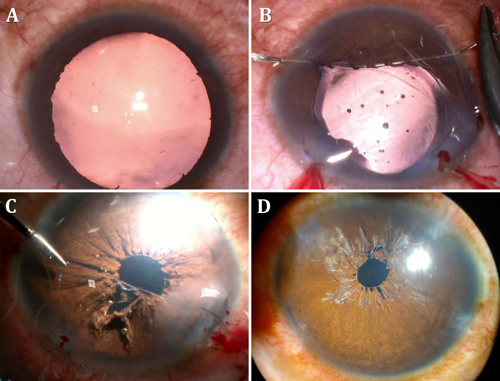
Blunt injury to the eye can result in traumatic mydriasis, secondary to localized or diffuse sphincter tears and can cause glare, photophobia, decreased visual acuity, as well as cosmetic concerns secondary to anisocoria. Both localized and diffuse sphincter damage may be managed with one or more pupilloplasty knots, as described in part two of this series. Diffuse sphincter dysfunction is better managed by iris cerclage, however. This procedure consists of a series of bites taken around the pupillary border in a drawstring fashion so that tightening the two ends of the sutures brings down the pupil size. This is done for a fixed and dilated pupil, generally from post-traumatic pathology or an atonic pupil.
Technique
Very often, the lens is cataractous from the previous trauma and cataract extraction with intraocular lens placement is done prior to iris cerclage. Non-cataractous eyes also require cataract extraction to avoid damage to the crystalline lens during needle passes.
Three limbal paracentesis incisions are made equidistant to each other, and the anterior chamber (AC) is filled with viscoelastic. The dilated iris tissue is pulled inwards gently using microforceps to bring down the pupillary aperture as much as possible. This helps prevent excess stretch and cheese-wiring of the iris later. Pulling the pupil inward is generally possible as iris stroma is relatively healthy in traumatic mydriasis and atonic pupils. With the iris maintained in this position, the AC is refilled with viscoelastic. A double-armed 10-0 Prolene suture with two long, thin, and curved needles (CI-4, Ethicon) on either end is used for iris cerclage.
First needle pass
The first needle is inserted through the paracentesis, taking care to avoid accidentally engaging corneal tissue. The needle is then weaved in and out multiple times close to the pupillary margin, starting from the paracentesis entry site and moving in one direction towards the adjacent paracentesis. The bites are taken such that the needle enters from the anterior stromal side, comes out from the posterior pigment epithelium side, and then similarly moves forward for the next bite—making the needle go around the pupil edge multiple times. This technique requires considerable ambidexterity: the first hand holding the needle needs to be equally assisted by the second hand moving the iris tissue and gently lifting it into position each time to pass the needle from the upper side to the underside of the iris and subsequently push the iris bites along the needle to enable more bites.
Once the needle nears the adjacent paracentesis, it is brought out carefully and gently—encouraged by gently pushing the multiple iris bites distally along the needle length with microforceps to enable the needle to pass through without any cheese-wiring. The needle is brought out by railroading it into a 27-gauge cannula passed through the paracentesis to prevent accidental engagement of corneal tissue at the paracentesis. Care should be taken so none of the above manoeuvres exert excess stress on the iris root to accidentally cause a dialysis. The suture is gently pulled out through the paracentesis before the needle is turned to enter again through the same paracentesis, this time directed toward the third paracentesis with the same procedure repeated carefully to bring the needle out. The AC is replenished with viscoelastic whenever required.
Second needle pass
The second needle of the double-armed suture is now grasped with a needle holder and inserted through the first paracentesis. It is passed multiple times through the pupil border in the opposite direction to the first needle’s path to exit through the third paracentesis. On drawing this needle out, the suture loop enters the AC, and on tightening, the suture encircles the pupil margin from both sides, with both needles having finally exited through the third paracentesis.
Tying the knot
The knot can be tied in one of two ways—using a modified McCannel technique as described by Dr Ike Ahmed, where one end of the suture is cut and looped a few times around a needle holder and tied to the second end. The cut end is then introduced into the AC and grabbed from the opposite paracentesis to cinch the knot. Pulling both ends tightens the drawstring suture around the pupil, thus bringing the pupil size down. Care should be taken not to over-tighten—a pupillary size of 3.5 mm–4.0 mm is ideal for visual purposes and to examine the retina later if required. A second knot may similarly lock the knot and prevent slippage.
The second technique to tie the knot is with the single-pass, four-throw technique, where one needle is internalized and railroaded into a cannula introduced from the opposite paracentesis to come out without taking any iris bite. This gives two sutures in opposite directions, one of which can then be looped out using a Sinskey hook and tied down with a single-pass, four-throw technique.
Running suture technique
This technique uses a long, thin needle on a polypropylene suture threaded along the iris near the pupillary border and then tied down to complete the cerclage.
Advantages
The iris cerclage suture is useful for diffuse sphincter damage where the iris stromal tissue is still healthy. It creates minimal focal stress on the pupil, avoids over-stretching of iris stroma, and gives a cosmetically appealing, round pupil that can be easily titrated to the desired size. Since the effect of the encerclage is like a drawstring, the pupil is centrally placed and not displaced, as can happen with other pupilloplasty techniques. It also effectively decreases glare and other photic phenomena the patient suffers from and helps improve visual acuity and quality by removing the effects of peripheral aberrations.
Disadvantages
It is more difficult to perform and has a longer learning curve. The needle has to travel a long distance, taking multiple bites near the pupillary edge—which can be time-consuming and require considerable manual dexterity. The suture can cheese-wire through the pupillary bites during this long pass or while pulling the needle out, leading to ‘dropped sections’ and areas where the suture traverses the AC between bites and the pupil remains focally dilated. In addition, the pupil is completely ‘locked’ to a particular size and cannot be dilated beyond since the prolene suture encircles it. This contrasts with a repair using two to three Siepser or single-pass, four-throw pupilloplasty knots to bring down the pupil size, leaving the pupil in between the knots untouched and still dilatable to an extent.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India, and can be reached at dr_soosanj@hotmail.com.