Cornea, Corneal Therapeutics
DSO Shows Promise in Treating Fuchs' Dystrophy
Improved results were seen with no rejection concerns.
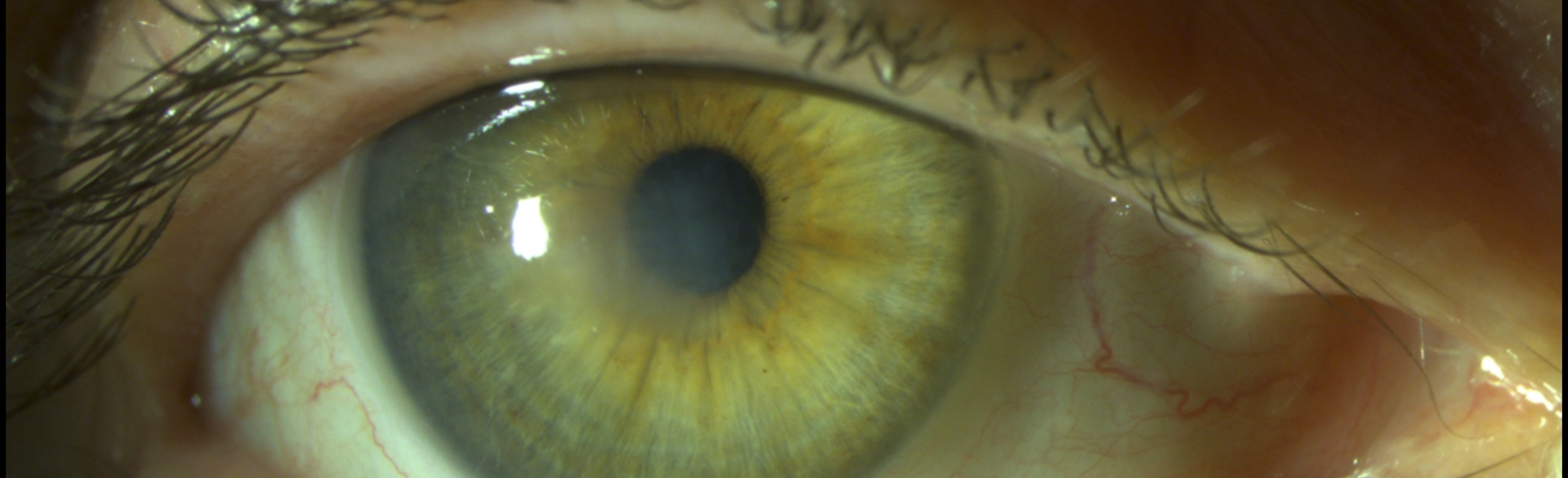
Impressive surgical advances have been made in Fuchs’ endothelial corneal dystrophy (FECD) treatment over the past 25 years, with ongoing insights into the biology and genetics of the disease potentially paving the way to an eventual medical therapy of the condition in our lifetime, according to Kathryn Colby MD, PhD.
Speaking at the EuCornea Congress in Paris, Dr Colby focused her presentation on the exciting possibilities of descemet stripping only (DSO) as a viable treatment for some patients with FECD.
“Over the past 25 years, we have seen a shift in the way we manage Fuchs’ dystrophy surgically,” she said. “We don’t do penetrating keratoplasty anymore, and 2023 was the first year in the United States that Descemet membrane endothelial keratoplasty (DMEK) actually exceeded the numbers of Descemet stripping automated endothelial keratoplasty (DSAEK) procedures for endothelial dysfunction. Since 2014, we have really ushered in the era of modern DSO for treating the disease with results that continue to improve.”
As with every surgical treatment, DSO has its advantages and downsides.
“DMEK is a wonderful surgery with quick visual recovery, but there is still a 6% rejection rate without steroids,” Dr Colby explained. “With DSO, there is no foreign tissue needed and therefore no rejection risk and no risks of long-term steroids. It is a straightforward surgical technique that removes central corneal guttae known to be visually significant.”
On the downside, DSO is not a universal treatment for all FECD cases.
“If the patient has limbus to limbus guttae, they will not do well with DSO. In our original series, we had about a 75% success rate. This was before the era of rho kinase inhibitor (ROCK) supplementation, and some series now approach 100%, but we are not quite there yet.”
Visual rehabilitation and durability of treatment also need to be considered, she said.


“We need to bear in mind that immediately [after] surgery, there will be worse vision after DSO. We remove the endothelium and Descemet membrane, so there will be corneal oedema. The duration of the effect is also not known. The remaining endothelial cells that repopulated the central cornea still have the disease. However, my index patient is now 10 years out from treatment and is still doing well.”
Dr Colby offered three tips to maximise outcomes from DSO treatments: patient selection, surgical technique, and ROCK inhibitor supplementation.
“Patients [need] to have predominantly central guttae with a preserved peripheral endothelial mosaic,” she said. “They [must] be able to tolerate reduced vision for three to six weeks after DSO, and they have to be willing to have an endothelial keratoplasty if the DSO is not successful.”
In surgical technique, Dr Colby advised removing as many of the central confluent guttae as possible but proceeding very gently with the surgery. “If you put a surgical hook into the posterior corneal stroma, you will cause scarring. Additionally, it is best to aim for a smooth-edged tear and to try to centre the descemetorhexis on the visual axis,” she said.
Finally, she advised using a ROCK inhibitor after DSO surgery. “Both ripasudil and netarsudil have been shown to speed corneal clearance and increase final endothelial cell count after DSO in investigator-initiated series.”
Ripasudil has already successfully completed a multinational phase II trial, with patients currently enrolling for randomised phase III trials with the aim of FDA approval.
Looking to the future, Dr Colby suggested DSO might be combined with new therapies for even better outcomes.
“We know the corneal guttae themselves are visually significant. DSO offers a nice option [for combination] with some new therapies that may improve endothelial cell function or reduce the continued dysfunction of the cells,” she said. “In development right now are a bio-engineered fibroblastic growth factor and small molecules which can inhibit the downstream effect of repeat expansion underlying the bulk of FECD.”

Kathryn Colby MD, PhD is the Elisabeth J Cohen Professor and Chairman of the Department of Ophthalmology at NYU Grossman School of Medicine, New York, US. Kathryn.Colby@nyulangone.org
Tags: cornea, FECD, Fuchs' dystrophy, DSO, descemet stripping only, DMEK, DSAEK, endothelial dysfunction, Kathryn Colby
Latest Articles
Organising for Success
Professional and personal goals drive practice ownership and operational choices.
Update on Astigmatism Analysis
Is Frugal Innovation Possible in Ophthalmology?
Improving access through financially and environmentally sustainable innovation.
iNovation Innovators Den Boosts Eye Care Pioneers
New ideas and industry, colleague, and funding contacts among the benefits.
José Güell: Trends in Cornea Treatment
Endothelial damage, cellular treatments, human tissue, and infections are key concerns on the horizon.
Making IOLs a More Personal Choice
Surgeons may prefer some IOLs for their patients, but what about for themselves?
Need to Know: Higher-Order Aberrations and Polynomials
This first instalment in a tutorial series will discuss more on the measurement and clinical implications of HOAs.
Never Go In Blind
Novel ophthalmic block simulator promises higher rates of confidence and competence in trainees.
Simulators Benefit Surgeons and Patients
Helping young surgeons build confidence and expertise.