COVID & the Eye
Ongoing research seeks possible ocular connections.

Howard Larkin
Published: Monday, February 1, 2021
 Since Li Wenliang MD first warned colleagues of a cluster of SARS-like pneumonia cases in late December 2019, ophthalmologists have been involved with COVID-19. Perhaps most urgently, Dr Li’s subsequent death from the disease, which he contracted from an asymptomatic glaucoma patient, dramatically illustrated the need for universal precautions to combat COVID-19 in clinical practice.
In the months since, ocular manifestations of SARS-CoV-2 infection and COVID-19 have been the subject of much study. One recent review estimated the pooled prevalence of ocular manifestations at 7%, with SARS-CoV-2 confirmed present on conjunctival swabs by PCR tests at about 1% (Taiwan J Ophthalmol.2020 Jul-Sep; 10(3): 153–166.).
However, other research suggests ocular involvement may be more common depending in part on how it is defined. For example, a standardised questionnaire of daily COVID-19 symptoms administered to patients served by hospitals in Strasbourg, Dijon, Nice, Brest and Colmar in France found that 36.7% reported ocular symptoms, and these were statistically associated with all major systemic manifestations, including flu-like illness, respiratory, neurological and digestive, said Tristan Bourcier MD, PhD, professor of ophthalmology at Strasbourg University Hospital.
“The symptoms reported by the patients resembled to a non-specific mild conjunctivitis confirming the possibility that SARS-CoV-2 targets ocular surface cells creating a potential entry portal. Moreover, SARS-CoV-2 has also been detected in the tears of COVID-19 patients suffering from conjunctivitis during illness,” said Dr Bourcier, who has been supporting patients with COVID-19 acute diseases along with ICU and infectious diseases colleagues since the pandemic entered France early last year.
But while COVID-19 anterior infections could theoretically trigger corneal graft rejections, uveitis or neuritis episodes, the reality is different, Dr Bourcier said. “Most of the COVID-19 patients suffer red eye and eyelid swelling with or without discharge. In the very majority of cases there is no visual impairment neither anatomical sequels.”
This observation coincides with the clinical experience of José Güell PhD, Professor of Ophthalmology at Autonoma University of Barcelona, Spain, and Director of Cornea and Refractive Surgery at IMO Barcelona. But while he has seen many cases of diffuse conjunctivitis in COVID-19 patients, and these cases are often referred to him, he has yet to see a conjunctival swab positive for the virus.
Because these patients also are exposed to other eye-drying circumstances, such as spending much more time looking at computer and smart phone screens, and staying indoors, “it is really difficult to assign the cause to COVID”, he said. Generally, these cases resemble a mild viral conjunctivitis and respond well to low-dose topical corticosteroids. He is much more concerned with the risk of contagion for the staff in treating patients.
Since Li Wenliang MD first warned colleagues of a cluster of SARS-like pneumonia cases in late December 2019, ophthalmologists have been involved with COVID-19. Perhaps most urgently, Dr Li’s subsequent death from the disease, which he contracted from an asymptomatic glaucoma patient, dramatically illustrated the need for universal precautions to combat COVID-19 in clinical practice.
In the months since, ocular manifestations of SARS-CoV-2 infection and COVID-19 have been the subject of much study. One recent review estimated the pooled prevalence of ocular manifestations at 7%, with SARS-CoV-2 confirmed present on conjunctival swabs by PCR tests at about 1% (Taiwan J Ophthalmol.2020 Jul-Sep; 10(3): 153–166.).
However, other research suggests ocular involvement may be more common depending in part on how it is defined. For example, a standardised questionnaire of daily COVID-19 symptoms administered to patients served by hospitals in Strasbourg, Dijon, Nice, Brest and Colmar in France found that 36.7% reported ocular symptoms, and these were statistically associated with all major systemic manifestations, including flu-like illness, respiratory, neurological and digestive, said Tristan Bourcier MD, PhD, professor of ophthalmology at Strasbourg University Hospital.
“The symptoms reported by the patients resembled to a non-specific mild conjunctivitis confirming the possibility that SARS-CoV-2 targets ocular surface cells creating a potential entry portal. Moreover, SARS-CoV-2 has also been detected in the tears of COVID-19 patients suffering from conjunctivitis during illness,” said Dr Bourcier, who has been supporting patients with COVID-19 acute diseases along with ICU and infectious diseases colleagues since the pandemic entered France early last year.
But while COVID-19 anterior infections could theoretically trigger corneal graft rejections, uveitis or neuritis episodes, the reality is different, Dr Bourcier said. “Most of the COVID-19 patients suffer red eye and eyelid swelling with or without discharge. In the very majority of cases there is no visual impairment neither anatomical sequels.”
This observation coincides with the clinical experience of José Güell PhD, Professor of Ophthalmology at Autonoma University of Barcelona, Spain, and Director of Cornea and Refractive Surgery at IMO Barcelona. But while he has seen many cases of diffuse conjunctivitis in COVID-19 patients, and these cases are often referred to him, he has yet to see a conjunctival swab positive for the virus.
Because these patients also are exposed to other eye-drying circumstances, such as spending much more time looking at computer and smart phone screens, and staying indoors, “it is really difficult to assign the cause to COVID”, he said. Generally, these cases resemble a mild viral conjunctivitis and respond well to low-dose topical corticosteroids. He is much more concerned with the risk of contagion for the staff in treating patients.
 Ashok Kumar PhD
Ashok Kumar PhD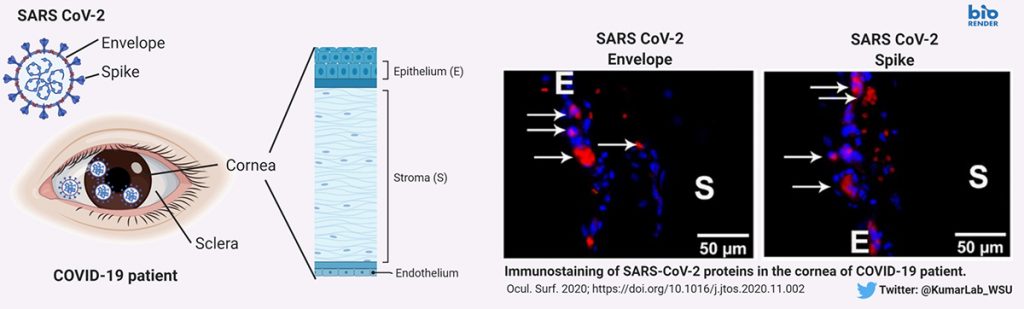 Schematic of corneal tissue indicating different layers and detection of SARS CoV-2 Spike and Envelope proteins in cornea of COVID-19 donor eyes
ROLE OF INFLAMMATION
While both the conjunctiva and the cornea express the ACE2 receptors and Furin protease required for SARS-CoV-2 to enter cells, it remains uncertain whether the ocular surface could be another entry route, Dr Kumar said. One of the unique aspects of his study is the presence of SARS-CoV-2 viral antigens (i.e., Spike and Envelope proteins) in the corneal epithelium of COVID-19 donor eyes. This provides a stronger evidence than viral RNA detection and suggest potential susceptibility of ocular surface cells to SARS-CoV-2 infection. With colleagues at the University of California – Los Angeles, USA, he is conducting a study involving mice that express human ACE2 on the cornea to see if they can contract systemic SARS-CoV-2 infections through the eye, establishing a theoretical animal model for this transmission route. They are also examining the virus’ effect on cultured human corneal epithelial cells, particularly the induction of antiviral and inflammatory responses. These experiments are needed to conclusively prove or refute whether eye is a gateway for SARS-CoV-2 entry – he further added.
Schematic of corneal tissue indicating different layers and detection of SARS CoV-2 Spike and Envelope proteins in cornea of COVID-19 donor eyes
ROLE OF INFLAMMATION
While both the conjunctiva and the cornea express the ACE2 receptors and Furin protease required for SARS-CoV-2 to enter cells, it remains uncertain whether the ocular surface could be another entry route, Dr Kumar said. One of the unique aspects of his study is the presence of SARS-CoV-2 viral antigens (i.e., Spike and Envelope proteins) in the corneal epithelium of COVID-19 donor eyes. This provides a stronger evidence than viral RNA detection and suggest potential susceptibility of ocular surface cells to SARS-CoV-2 infection. With colleagues at the University of California – Los Angeles, USA, he is conducting a study involving mice that express human ACE2 on the cornea to see if they can contract systemic SARS-CoV-2 infections through the eye, establishing a theoretical animal model for this transmission route. They are also examining the virus’ effect on cultured human corneal epithelial cells, particularly the induction of antiviral and inflammatory responses. These experiments are needed to conclusively prove or refute whether eye is a gateway for SARS-CoV-2 entry – he further added.
 Sezen Karakus MD
Sezen Karakus MD