CANALOPLASTY UPDATE
Medium-term canaloplasty results show sustained IOP reduction
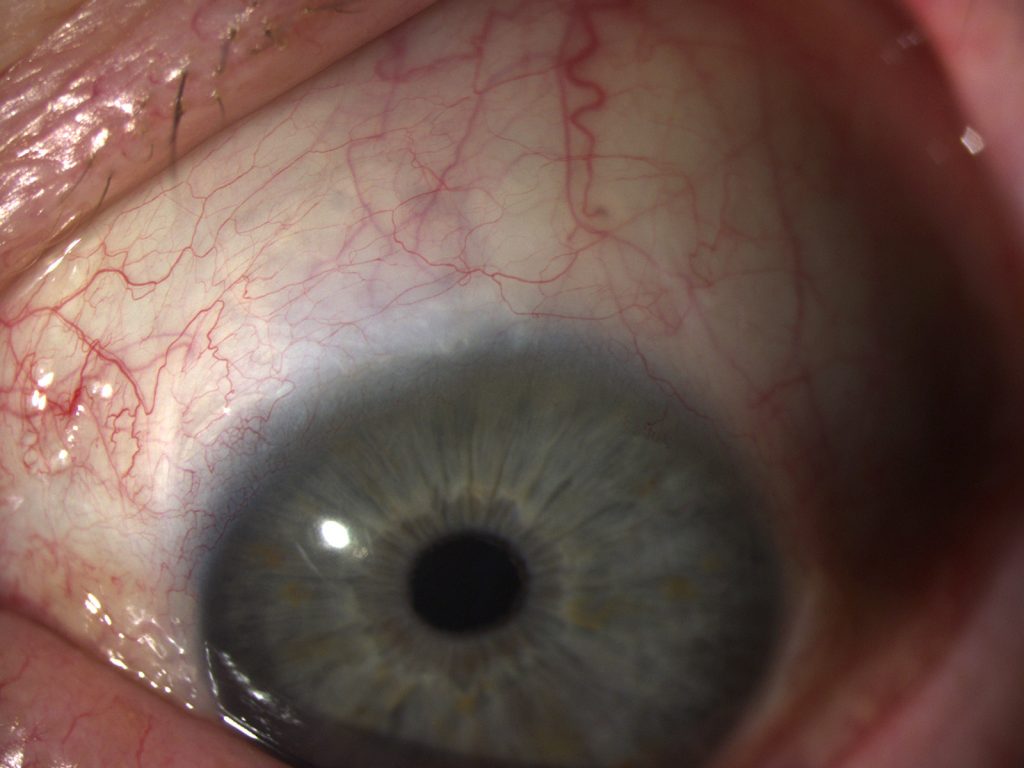
Slit-lamp photograph of an eye with refractory pseudoexfoliation glaucoma, four years after canaloplasty. Courtesy of Paolo Santorum MD.
Ab externo canaloplasty is safe and effective in lowering intraocular pressure in eyes with refractory open-angle glaucoma, with more than a third of patients who undergo the procedure likely to remain drop-free four years after surgery, said Paolo Santorum MD, San Maurizio Regional Hospital, Bolzano, Italy.
“Ab externo canaloplasty has an efficacy similar to that of trabeculectomy but with a better safety profile,” Dr Santorum told the XXXV Congress of the ESCRS in Lisbon, Portugal.
COMPARATIVE STUDY
He presented a retrospective case series study that compared 58 eyes that underwent canaloplasty with 89 eyes that underwent trabeculectomy with mitomycin-C for primary open-angle glaucoma, pigmentary glacuoma or pseudoexfoliation glaucoma during the years 2011 to 2017.
Dr Santorum and his associates defined complete success as not needing a major reoperation or medication to control the intraocular pressure (IOP), and qualified success as not needing a major reoperation to control the IOP. Laser suture lysis, bleb-needling and suture of bleb-leakage procedures were not considered reoperations.
He noted that Kaplan-Meier survival analysis showed that, four years after surgery, canaloplasty-treated eyes had a 39% probability of complete success, and a 96% probability of qualified success. In comparison, trabeculectomy-treated eyes had a 15% probability of complete success and an 81% probability of qualified success, although the differences between the groups were not significant.
On the other hand, only six additional interventions were performed in the canaloplasty group, whereas 44 were necessary in the trabeculectomy group.
POSTOPERATIVE INTERVENTIONS
The postoperative interventions in the canaloplasty group were two sutures of inadvertently formed leaking bleb, two reoperations for high IOP, one hyphaema wash-out and one-cutting of the canal suture because of a flat anterior chamber.
Postoperative interventions in the trabeculectomy group included 16 laser suture lyses, six reoperations for hypotony, five bleb needlings, four reoperations for high IOP, three sutures of leaking bleb, three viscoelastic refills and three conjunctival cyst removals.
Dr Santorum emphasised that, although ab externo canaloplasty is not a minimally invasive surgery, it has several advantages over trabeculectomy. They include a lower risk of hypotony, a shorter hospital stay and a more easily managed postoperative course. In addition, canaloplasty leaves the patient with a more normal looking and physiologically natural eye. (Figure 1 and 2)
However, unlike trabeculectomy, canaloplasty cannot bring IOP any lower than the episcleral venous pressure. Therefore, canaloplasty is not recommended in eyes with a very low target IOP, Dr Santorum said.
Paolo Santorum: psantorum@gmail.com
Authors
Roibeard O’hEineachain
Published
Wednesday, January 30, 2019
Category