When posterior capsule rupture strikes
Preparation is key in tackling PCR during cataract surgery

Dermot McGrath
Published: Monday, February 1, 2021
 Sharp edge to capsular break
Sharp edge to capsular break Scalloped edge to capsular break
Scalloped edge to capsular break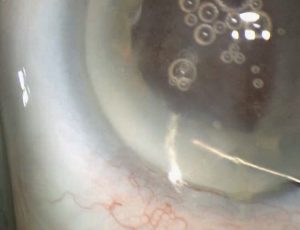 Residual vitreous exposed
Residual vitreous exposed