Treating hydrops
New surgical techniques make acute hydrops in keratoconus a treatable disease

Roibeard O’hEineachain
Published: Saturday, June 6, 2020
 Prof Bjӧrn Bachmann MD PhD FEBO
Prof Bjӧrn Bachmann MD PhD FEBO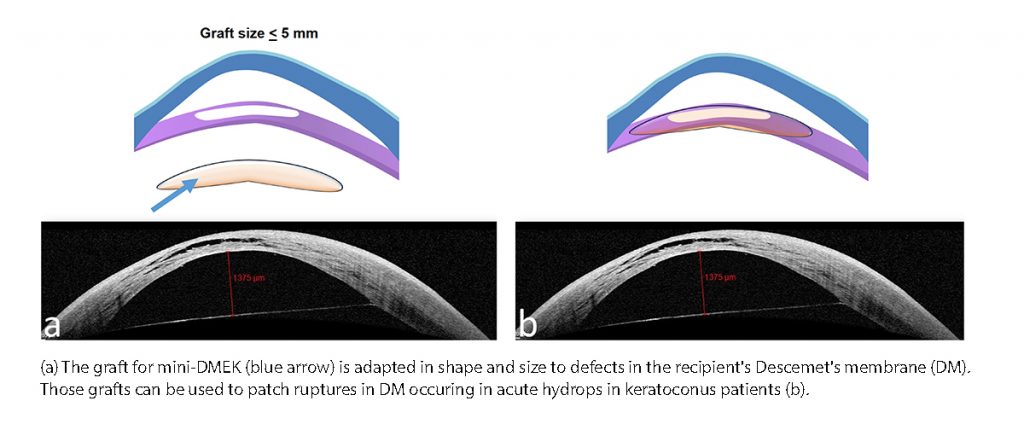 Mini-DMEK
A new approach in acute hydrops is the use of mini-DMEK grafts, sized 5.0mm or less, to patch the disrupted Descemet’s membrane. In a study he and his associates performed, four mini-DMEK procedures in three eyes of three patients, UCVA logMAR improved from 1.6 before to 1.2 after six-to-eight weeks. They had to repeat the procedure in one patient because the Descemet’s membrane of patient had so much tension the patch did not attach. They removed a piece of Descemet’s membrane from that patient. There was a partial detachment of graft without relapse of hydrops in two eyes.
Comparing Mini-DMEK vs compression sutures, Dr Bachmann noted that mini-DMEK has the advantage of eliminating any risk of suture loosening and leakage from the stitch canal. In addition. unlike compression sutures, mini-DMEK can treat massive oedema. Its main disadvantages are that it requires general anaesthesia and is a complex technique best performed with intraoperative optical coherence tomography (OCT). The main advantages of compression sutures are that it is an easy technique requiring no special equipment and can be performed with local anaesthesia. The main disadvantages with the technique are the risk of leakage and the risk of relapse in eyes with large amounts of oedema.
“Acute hydrops has become a treatable disease. In most patients surgical approaches rather than a purely conservative treatment is advisable. The new surgical treatments provide a rapid improvement in visual acuity and presumably results in less scar formation or vascularisation of the corneal stroma and reduce the risk of requiring a penetrating keratoplasty,” Prof Bachmann concluded.
Mini-DMEK
A new approach in acute hydrops is the use of mini-DMEK grafts, sized 5.0mm or less, to patch the disrupted Descemet’s membrane. In a study he and his associates performed, four mini-DMEK procedures in three eyes of three patients, UCVA logMAR improved from 1.6 before to 1.2 after six-to-eight weeks. They had to repeat the procedure in one patient because the Descemet’s membrane of patient had so much tension the patch did not attach. They removed a piece of Descemet’s membrane from that patient. There was a partial detachment of graft without relapse of hydrops in two eyes.
Comparing Mini-DMEK vs compression sutures, Dr Bachmann noted that mini-DMEK has the advantage of eliminating any risk of suture loosening and leakage from the stitch canal. In addition. unlike compression sutures, mini-DMEK can treat massive oedema. Its main disadvantages are that it requires general anaesthesia and is a complex technique best performed with intraoperative optical coherence tomography (OCT). The main advantages of compression sutures are that it is an easy technique requiring no special equipment and can be performed with local anaesthesia. The main disadvantages with the technique are the risk of leakage and the risk of relapse in eyes with large amounts of oedema.
“Acute hydrops has become a treatable disease. In most patients surgical approaches rather than a purely conservative treatment is advisable. The new surgical treatments provide a rapid improvement in visual acuity and presumably results in less scar formation or vascularisation of the corneal stroma and reduce the risk of requiring a penetrating keratoplasty,” Prof Bachmann concluded.