Cataract and MIGS
Part three in our series on everything you ever wanted to know about management of co-existing cataract and glaucoma

Soosan Jacob
Published: Tuesday, December 24, 2019
 Invasive glaucoma surgeries such as trabeculectomy, tube shunts and non-penetrating glaucoma surgeries have traditionally been reserved for patients with moderate-to-advanced glaucomas because of greater risks associated with them. Mild glaucoma is generally treated with medications or lasers, though poor compliance to medications, toxicity of preservatives and costs have always been issues.
For cataract patients with co-existent early-to-moderate glaucoma, minimally invasive glaucoma surgery (MIGS) is an option that has recently become more and more popular as despite lesser efficacy compared to traditional glaucoma surgeries, high safety profile is an advantage.
Other advantages include ease and minimally traumatic nature of surgery, early recovery, relative lack of major complications, possibility for effective and long-lasting IOP control with decreased number of medications together with ability to incorporate these techniques easily into one’s cataract practice.
Inclusion of many MIGS procedures under insurance has also gone towards making this a popular glaucoma treatment, especially when coexistent with cataract.
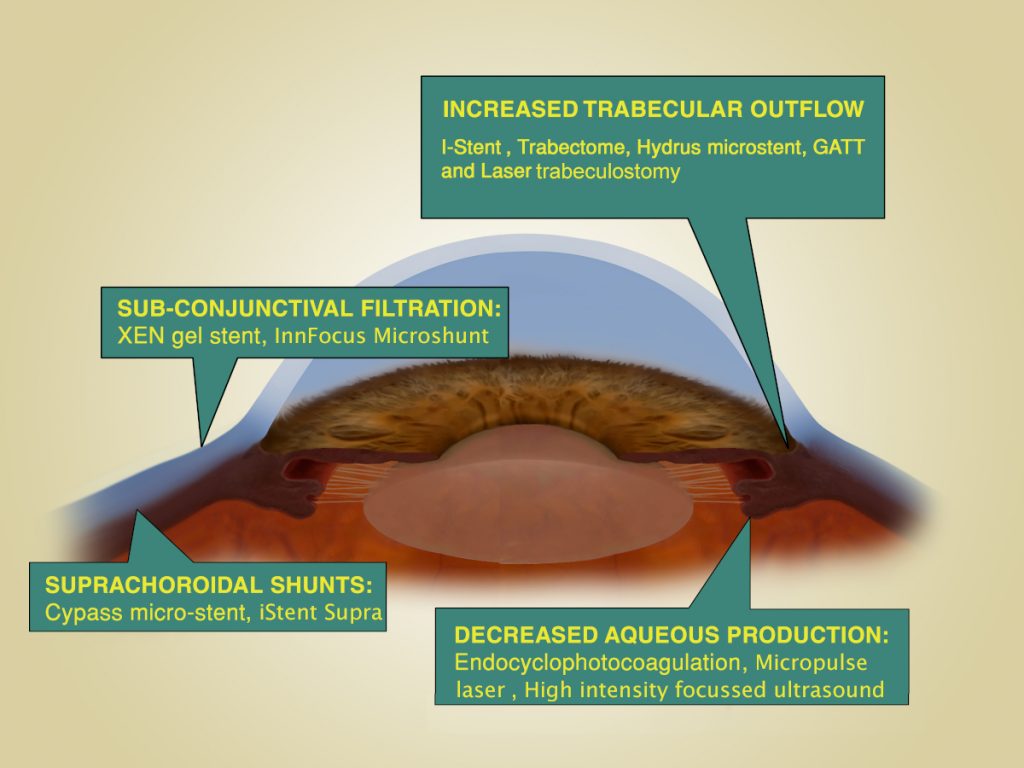
MIGS includes implants, devices and techniques. Most use an ab-interno conjunctiva- sparing approach, thus leaving virgin conjunctiva for any future glaucoma surgeries if required. Some, however, do affect the conjunctiva, such as the Aquesys Xen implant. MIGS can be classified depending on their mechanism of action:
I. INCREASED TRABECULAR OUTFLOW/ TRABECULAR BYPASS:
iStent (Glaukos Corp): This is a self-retaining, heparin-coated titanium stent with a pointed tip that penetrates through the trabecular meshwork for implantation into the Schlemm’s canal. Though overall mean IOP was similar to a control group at 24 months, there appears to be some benefit of stent implantation. Implantation of two stents was reported to give a 43% reduction in mean intraocular pressure (IOP) to 14.6mmHg up to 36 months’ follow-up.
The infero-nasal quadrants have a higher density of collector channels and may be preferred for implantation. The iStent Inject delivers with a single entry, two pre-loaded trabecular micro-bypass stents that can be implanted two-to-three clock hours apart.
The Hydrus microstent (Ivantis Inc) is an 8mm long curved device made from nitinol that is implanted via a pre-loaded injector. It provides an intra-canalicular scaffold to one quadrant of the Schlemm’s canal, dilates the canal by four-to-five times the natural width and prevents collapse of Schlemm’s canal secondary to elevated IOP. The device has windows that allow aqueous outflow.
A prospective, multi-centre, randomised controlled trial comparing one Hydrus device versus two iStents (COMPARE study) reported the Hydrus group to have a greater reduction in mean IOP than the iStent group (-1.7 vs. -1.0mmHg), though not reaching statistical significance. The Hydrus group showed superiority in certain other parameters as well.
The Trabectome (NeoMedix) performs an ab interno trabeculotomy and removes a strip of trabecular meshwork (TBM) and inner wall of Schlemm’s canal. The handpiece has irrigation, aspiration and electrocautery modes. A 60-to-120-degree ablation is generally performed. Advantages include conjunctival sparing, reasonable efficacy, absence of bleb and ability to combine with cataract surgery. Disadvantages include lack of flow all 360 degrees around, closure of the trabeculotomy, limitation by inherent episcleral venous pressure and Schlemm’s canal resistance.
Gonioscopy-assisted transluminal trabeculotomy (GATT)/ ab interno canaloplasty (ABiC): This ab interno technique has eliminated many of the disadvantages of ab externo trabeculotomy while retaining advantages of a 360-degree trabeculotomy/viscodilatation. Either the iTrack microcatheter (Ellex) with a 250-micron diameter or a 5-0 nylon/ prolene suture, the leading edge rounded by low temperature cautery, is advanced through the Schlemm’s canal 360 degrees circumferentially via an internal goniotomy incision. Viscodilatation (360 degrees) is performed in ABiC while suture/the microcatheter is tightened to create a 360-degree trabeculotomy in GATT. The illuminated tip of the iTrack helps guide the catheter reliably.
Excimer laser trabeculostomy is performed with a goniolens or endoscope and uses a fibre-optic-delivered 308‑nm xenon chloride excimer laser to create multiple (four-to-10) small ostia through the trabecular meshwork, juxtacanalicular trabecular meshwork and the inner wall of Schlemm’s canal via a non-thermal approach to improve outflow. It uses a clear corneal incision, sparing conjunctiva, thus minimising healing response that could otherwise close the ostia.
II. SUPRACHOROIDAL SHUNTS:
The iStent Supra (Glaukos Corp) is a 4mm tubular device made of polyethersulfone and titanium with a 160–170mm lumen. It also drains into the suprachoroidal space and is inserted ab interno. The Gold Shunt (SOLX Inc) and the STARflo (iSTAR Medical) are ab externo supraciliary implants placed under scleral flaps.
III. SUB-CONJUNCTIVAL FILTRATION:
Two devices – the XEN gel stent (AqueSys Implant) and the InnFocus Microshunt (InnFocus) are available for sub-conjunctival filtration. They are designed using Newtonian fluid dynamics and the Hagen–Poiseuille equation to eliminate clinically significant postoperative hypotony. Both have high biocompatibility and resist neovascularisation and fibrosis.
However, both are generally used together with anti-metabolites like 5-FU or Mitomycin-C. The XEN gel stent is made of soft, non-inflammatory porcine collagen-derived gelatin cross-linked with glutaraldehyde. It is 6mm in length and comes pre-loaded in three different internal lumen diameters – 140, 63 and 45 microns. It is implanted either completely ab interno or with conjunctival dissection. The InnFocus Microshunt is an 8.5mm long, flexible tube with a 70-micron lumen made of SIBS (synthetic Poly(Styrene-block-IsoButylene-block-Styrene)). It is inserted into the AC under a scleral flap and tiny fins on either side prevent it from migrating. It may be as effective as trabeculectomy and thus may be used for moderate-to-advanced glaucoma.
IV. DECREASED AQUEOUS PRODUCTION:
Endocyclophotocoagulation decreases aqueous production and has been combined with phacoemulsification since 1995. Micropulse cyclodiode laser (Iridex) uses ultra-short energy bursts, allowing tissue to cool between pulses thus minimizing damage. High-intensity focused ultrasound (Eye Tech Care) may also be used for decreasing aqueous production.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India and can be reached at dr_soosanj@hotmail.com
Invasive glaucoma surgeries such as trabeculectomy, tube shunts and non-penetrating glaucoma surgeries have traditionally been reserved for patients with moderate-to-advanced glaucomas because of greater risks associated with them. Mild glaucoma is generally treated with medications or lasers, though poor compliance to medications, toxicity of preservatives and costs have always been issues.
For cataract patients with co-existent early-to-moderate glaucoma, minimally invasive glaucoma surgery (MIGS) is an option that has recently become more and more popular as despite lesser efficacy compared to traditional glaucoma surgeries, high safety profile is an advantage.
Other advantages include ease and minimally traumatic nature of surgery, early recovery, relative lack of major complications, possibility for effective and long-lasting IOP control with decreased number of medications together with ability to incorporate these techniques easily into one’s cataract practice.
Inclusion of many MIGS procedures under insurance has also gone towards making this a popular glaucoma treatment, especially when coexistent with cataract.
MIGS includes implants, devices and techniques. Most use an ab-interno conjunctiva- sparing approach, thus leaving virgin conjunctiva for any future glaucoma surgeries if required. Some, however, do affect the conjunctiva, such as the Aquesys Xen implant. MIGS can be classified depending on their mechanism of action:
I. INCREASED TRABECULAR OUTFLOW/ TRABECULAR BYPASS:
iStent (Glaukos Corp): This is a self-retaining, heparin-coated titanium stent with a pointed tip that penetrates through the trabecular meshwork for implantation into the Schlemm’s canal. Though overall mean IOP was similar to a control group at 24 months, there appears to be some benefit of stent implantation. Implantation of two stents was reported to give a 43% reduction in mean intraocular pressure (IOP) to 14.6mmHg up to 36 months’ follow-up.
The infero-nasal quadrants have a higher density of collector channels and may be preferred for implantation. The iStent Inject delivers with a single entry, two pre-loaded trabecular micro-bypass stents that can be implanted two-to-three clock hours apart.
The Hydrus microstent (Ivantis Inc) is an 8mm long curved device made from nitinol that is implanted via a pre-loaded injector. It provides an intra-canalicular scaffold to one quadrant of the Schlemm’s canal, dilates the canal by four-to-five times the natural width and prevents collapse of Schlemm’s canal secondary to elevated IOP. The device has windows that allow aqueous outflow.
A prospective, multi-centre, randomised controlled trial comparing one Hydrus device versus two iStents (COMPARE study) reported the Hydrus group to have a greater reduction in mean IOP than the iStent group (-1.7 vs. -1.0mmHg), though not reaching statistical significance. The Hydrus group showed superiority in certain other parameters as well.
The Trabectome (NeoMedix) performs an ab interno trabeculotomy and removes a strip of trabecular meshwork (TBM) and inner wall of Schlemm’s canal. The handpiece has irrigation, aspiration and electrocautery modes. A 60-to-120-degree ablation is generally performed. Advantages include conjunctival sparing, reasonable efficacy, absence of bleb and ability to combine with cataract surgery. Disadvantages include lack of flow all 360 degrees around, closure of the trabeculotomy, limitation by inherent episcleral venous pressure and Schlemm’s canal resistance.
Gonioscopy-assisted transluminal trabeculotomy (GATT)/ ab interno canaloplasty (ABiC): This ab interno technique has eliminated many of the disadvantages of ab externo trabeculotomy while retaining advantages of a 360-degree trabeculotomy/viscodilatation. Either the iTrack microcatheter (Ellex) with a 250-micron diameter or a 5-0 nylon/ prolene suture, the leading edge rounded by low temperature cautery, is advanced through the Schlemm’s canal 360 degrees circumferentially via an internal goniotomy incision. Viscodilatation (360 degrees) is performed in ABiC while suture/the microcatheter is tightened to create a 360-degree trabeculotomy in GATT. The illuminated tip of the iTrack helps guide the catheter reliably.
Excimer laser trabeculostomy is performed with a goniolens or endoscope and uses a fibre-optic-delivered 308‑nm xenon chloride excimer laser to create multiple (four-to-10) small ostia through the trabecular meshwork, juxtacanalicular trabecular meshwork and the inner wall of Schlemm’s canal via a non-thermal approach to improve outflow. It uses a clear corneal incision, sparing conjunctiva, thus minimising healing response that could otherwise close the ostia.
II. SUPRACHOROIDAL SHUNTS:
The iStent Supra (Glaukos Corp) is a 4mm tubular device made of polyethersulfone and titanium with a 160–170mm lumen. It also drains into the suprachoroidal space and is inserted ab interno. The Gold Shunt (SOLX Inc) and the STARflo (iSTAR Medical) are ab externo supraciliary implants placed under scleral flaps.
III. SUB-CONJUNCTIVAL FILTRATION:
Two devices – the XEN gel stent (AqueSys Implant) and the InnFocus Microshunt (InnFocus) are available for sub-conjunctival filtration. They are designed using Newtonian fluid dynamics and the Hagen–Poiseuille equation to eliminate clinically significant postoperative hypotony. Both have high biocompatibility and resist neovascularisation and fibrosis.
However, both are generally used together with anti-metabolites like 5-FU or Mitomycin-C. The XEN gel stent is made of soft, non-inflammatory porcine collagen-derived gelatin cross-linked with glutaraldehyde. It is 6mm in length and comes pre-loaded in three different internal lumen diameters – 140, 63 and 45 microns. It is implanted either completely ab interno or with conjunctival dissection. The InnFocus Microshunt is an 8.5mm long, flexible tube with a 70-micron lumen made of SIBS (synthetic Poly(Styrene-block-IsoButylene-block-Styrene)). It is inserted into the AC under a scleral flap and tiny fins on either side prevent it from migrating. It may be as effective as trabeculectomy and thus may be used for moderate-to-advanced glaucoma.
IV. DECREASED AQUEOUS PRODUCTION:
Endocyclophotocoagulation decreases aqueous production and has been combined with phacoemulsification since 1995. Micropulse cyclodiode laser (Iridex) uses ultra-short energy bursts, allowing tissue to cool between pulses thus minimizing damage. High-intensity focused ultrasound (Eye Tech Care) may also be used for decreasing aqueous production.
Dr Soosan Jacob is Director and Chief of Dr Agarwal’s Refractive and Cornea Foundation at Dr Agarwal’s Eye Hospital, Chennai, India and can be reached at dr_soosanj@hotmail.com