Artificial intelligence: Retina and beyond
The future is now: exciting potential of artificial intelligence applications in ophthalmology

Dermot McGrath
Published: Saturday, June 1, 2019
 Close-up of an OCT machine performing a scan. Image courtesy of Pearse A.Keane,MD,FRCOpth
Deep learning and advanced artificial intelligence (AI) applications hold exciting potential in diagnosing and treating a wide range of eye diseases and are already making an impact on current clinical practice, according to Adnan Tufail MBBS, MD, FRCOphth.
“There is little doubt that AI is probably at the peak of the famous hype curve at the moment and everybody from big pharma to the retinal physician wants to be a part of the revolution,” he told delegates attending the 18th EURETINA Congress in Vienna.
The current AI hype is being driven by the confluence of deep learning algorithms, massive datasets and powerful and relatively inexpensive computers, said Dr Tufail.
“The difference now is that we’re no longer talking about this in the future tense – the technology is already with us, even though we may not be aware of it,” he said.
Examples of current AI applications include Warren Hill’s online biometry formula, which uses neural networking to approximate IOL power based on input parameters, pattern recognition and machine learning, visual field progression models using machine learning and several diabetic retinopathy (DR) screening programmes that use a deep learning approach.
VALIDATION ISSUES
With regulatory authorities struggling to keep up with the rapid development of AI healthcare applications, independent validation is important for large-scale deployment of such algorithms, said Dr Tufail.
One such validation project in the United Kingdom recently tested a number of automated retinal analysis systems for DR using data from more than 20,000 patients and more than 100,000 images. Two of the four systems tested, Retmarker and EyeArt, achieved acceptable sensitivity for referable retinopathy and false-positive rates compared with human graders as reference standard.
“The fastest of these algorithms is capable of processing 600,000 images a day, which would save the National Health Service (NHS) around £10 million a year compared to manual grading,” he said.
Other interesting developments on the horizon include the integration of machine learning software into specialised devices, such as the home-screening OCT system currently being developed by Peter Maloca at the University of Bern, Switzerland, as well as surgical robotic systems with advanced AI capability.
Although there is understandable anxiety about the role of technology in day-to-day practice, Dr Tufail said that the benefits will ultimately far outweigh the risks.
“It will definitely impact on our working practices for screening, referral, diagnostic support, to detect abnormalities beyond the human range, and help us to manage clinic flow better. The bottom line is that AI is not going to put us out of a job, but we need to embrace this technology to make us the best retinal specialists that we can possibly be,” he said.
[caption id="attachment_15272" align="alignleft" width="1024"]
Close-up of an OCT machine performing a scan. Image courtesy of Pearse A.Keane,MD,FRCOpth
Deep learning and advanced artificial intelligence (AI) applications hold exciting potential in diagnosing and treating a wide range of eye diseases and are already making an impact on current clinical practice, according to Adnan Tufail MBBS, MD, FRCOphth.
“There is little doubt that AI is probably at the peak of the famous hype curve at the moment and everybody from big pharma to the retinal physician wants to be a part of the revolution,” he told delegates attending the 18th EURETINA Congress in Vienna.
The current AI hype is being driven by the confluence of deep learning algorithms, massive datasets and powerful and relatively inexpensive computers, said Dr Tufail.
“The difference now is that we’re no longer talking about this in the future tense – the technology is already with us, even though we may not be aware of it,” he said.
Examples of current AI applications include Warren Hill’s online biometry formula, which uses neural networking to approximate IOL power based on input parameters, pattern recognition and machine learning, visual field progression models using machine learning and several diabetic retinopathy (DR) screening programmes that use a deep learning approach.
VALIDATION ISSUES
With regulatory authorities struggling to keep up with the rapid development of AI healthcare applications, independent validation is important for large-scale deployment of such algorithms, said Dr Tufail.
One such validation project in the United Kingdom recently tested a number of automated retinal analysis systems for DR using data from more than 20,000 patients and more than 100,000 images. Two of the four systems tested, Retmarker and EyeArt, achieved acceptable sensitivity for referable retinopathy and false-positive rates compared with human graders as reference standard.
“The fastest of these algorithms is capable of processing 600,000 images a day, which would save the National Health Service (NHS) around £10 million a year compared to manual grading,” he said.
Other interesting developments on the horizon include the integration of machine learning software into specialised devices, such as the home-screening OCT system currently being developed by Peter Maloca at the University of Bern, Switzerland, as well as surgical robotic systems with advanced AI capability.
Although there is understandable anxiety about the role of technology in day-to-day practice, Dr Tufail said that the benefits will ultimately far outweigh the risks.
“It will definitely impact on our working practices for screening, referral, diagnostic support, to detect abnormalities beyond the human range, and help us to manage clinic flow better. The bottom line is that AI is not going to put us out of a job, but we need to embrace this technology to make us the best retinal specialists that we can possibly be,” he said.
[caption id="attachment_15272" align="alignleft" width="1024"]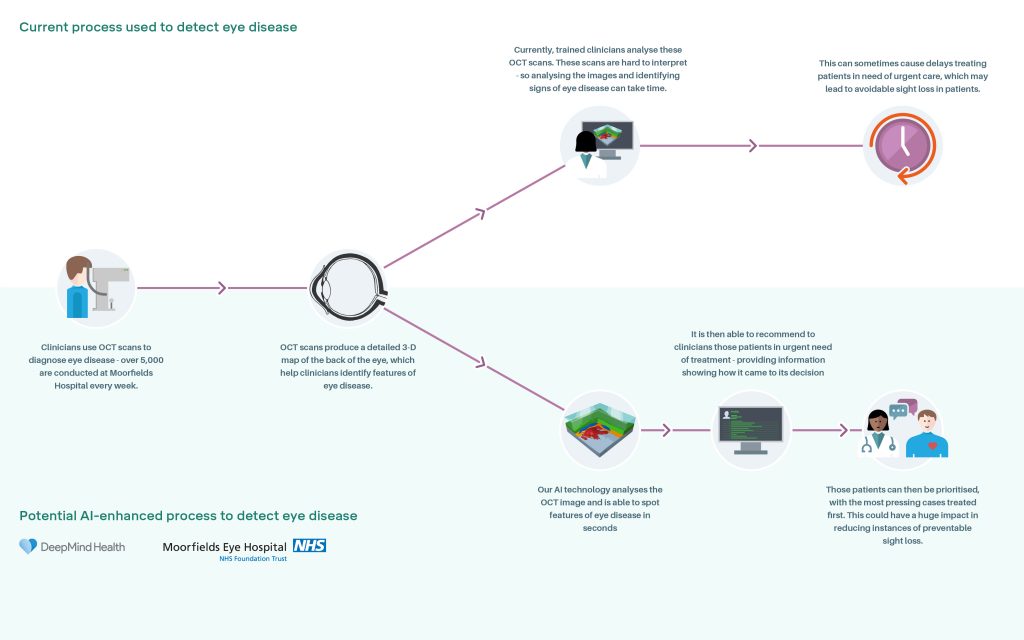 Click to enlarge[/caption]
REVOLUTIONARY AI SYSTEM
In a separate presentation, Pearse A. Keane MD, FRCOphth, gave an update on a potentially revolutionary AI system developed by researchers at Moorfields Eye Hospital NHS Foundation Trust, DeepMind and University College London (UCL) Institute of Ophthalmology.
“The system can recommend the correct referral decision for a wide range of eye diseases such as age-related macular degeneration and diabetic eye disease as accurately as world-leading experts,” said Dr Keane.
Using two types of neural network – mathematical systems for identifying patterns in images or data – the AI system quickly learnt to identify 10 features of eye disease from highly complex optical coherence tomography (OCT) scans. It was then able to recommend a referral decision based on the most urgent conditions detected.
“The system gives us a huge amount of quantitative information from the scans. It then makes a referral decision – urgent, semi-urgent, routine referral or observation only, as well as diagnosing the different disease categories. We have trained this algorithm on more than 50 different types of retinal diseases,” said Dr Keane.
The algorithm can, for instance, recognise choroidal neovascularisation (CNV), not only in the context of wet AMD, but also in the context of myopia, inflammatory CNV, central serous retinopathy (CSR) and so forth. Similarly with macular oedema, it can recognise diabetic macular oedema, macular oedema stemming from uveitis and other subtypes, he said.
Click to enlarge[/caption]
REVOLUTIONARY AI SYSTEM
In a separate presentation, Pearse A. Keane MD, FRCOphth, gave an update on a potentially revolutionary AI system developed by researchers at Moorfields Eye Hospital NHS Foundation Trust, DeepMind and University College London (UCL) Institute of Ophthalmology.
“The system can recommend the correct referral decision for a wide range of eye diseases such as age-related macular degeneration and diabetic eye disease as accurately as world-leading experts,” said Dr Keane.
Using two types of neural network – mathematical systems for identifying patterns in images or data – the AI system quickly learnt to identify 10 features of eye disease from highly complex optical coherence tomography (OCT) scans. It was then able to recommend a referral decision based on the most urgent conditions detected.
“The system gives us a huge amount of quantitative information from the scans. It then makes a referral decision – urgent, semi-urgent, routine referral or observation only, as well as diagnosing the different disease categories. We have trained this algorithm on more than 50 different types of retinal diseases,” said Dr Keane.
The algorithm can, for instance, recognise choroidal neovascularisation (CNV), not only in the context of wet AMD, but also in the context of myopia, inflammatory CNV, central serous retinopathy (CSR) and so forth. Similarly with macular oedema, it can recognise diabetic macular oedema, macular oedema stemming from uveitis and other subtypes, he said.
 Pearse Keane, consultant ophthalmologist,
analysing an OCT scan (top)
Pearse Keane, consultant ophthalmologist,
analysing an OCT scan (top)