Preloaded Tissue Changing the Face of Transplant Surgery
Eye banks of the future draw nearer as technological advances strengthen surgeon skill. Dermot McGrath reports.

Dermot McGrath
Published: Thursday, December 1, 2022
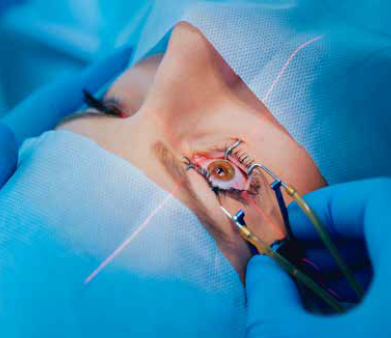
Using pre-cut and preloaded donor graft tissue for endothelial keratoplasty (EK) can significantly reduce operating time, minimise intraoperative tissue manipulation, and facilitate access to EK procedures for less experienced surgeons, according to Stefano Ferrari PhD.
“We have seen a major evolution in recent years with the shift from full-graft penetrating keratoplasty (PK) procedures towards selective lamellar and endothelial procedures. This has led to an increased demand for eye bank prepared and preloaded tissues for Descemet stripping automated endothelial keratoplasty (DSAEK) and Descemet membrane endothelial keratoplasty (DMEK),” he said.
Speaking to EuroTimes, Dr Ferrari said there are several advantages to using preloaded tissue from eye banks.
“The first advantage is the reduction in surgery time, as the surgeon no longer has to prepare the tissue in the operating room,” he explained. “In many hospitals in Italy, there is a specific time slot allocated for the use of the surgery room. Sometimes the ophthalmology department has its own surgery room, but often they need to use shared platforms and all the ophthalmology procedures have to be performed in an allocated amount of time. So, it stands to reason that if you reduce the time of every single procedure, then you can perform more procedures in the same amount of time.”
The next clear benefit of using preloaded tissue is it significantly reduces the learning curve for surgeons who perform only occasional corneal transplants and for whom the more technically challenging DMEK procedure can be daunting.
“The learning curve of DMEK procedure is quite steep, and the more cases you do, the better you become. But it remains technically difficult, and preparing the tissue is stressful for many surgeons,” Dr Ferrari remarked. “By contrast, our technicians in the eye bank prepare up to 10 tissues for DMEK or DSAEK a day, so they have perfected their skills over time. This is another advantage—because the technicians are so used to performing the tasks, the quality of the tissue is much better.”
Having preloaded tissue also removes the risk of stripping Descemet’s membrane in the operating room and compromising the surgery if not performed correctly.
“It is a delicate procedure and a lot can potentially go wrong when stripping the endothelium. This can mean a postponed surgery and a wasted cornea. And even if you have a backup cornea, there is obviously an extra cost involved in having to use that as well. Having the tissue ready to be transplanted makes life a lot easier and reduces a lot of the stress for the surgeon,” he said.
With demand increasing for preloaded tissue, Dr Ferrari believes better delivery devices and storage techniques will continue to drive improved efficiency and outcomes in the future.
“There are a lot of different delivery systems currently available for graft delivery in DMEK, for instance, but none of them are optimal in all aspects of the procedure. We need better and smoother delivery methods, more transparency for easier handling, and greater visibility during the graft transfer.
There are many issues that can be improved to make the devices even better,” he said.
Dr Ferrari believes the eye bank of the near future will also evolve to take account of advances in bioengineering and cellular technologies.
“I can see eye bank services expanding to the point where we have laboratories incorporated that work with cells as well as tissues. So, eye banks will offer cellular therapies under good manufacturing practices (GMP) where cells can be amplified and manipulated for transplantation—or artificial corneas for patients with advanced keratoconus. There are so many possibilities, and it’s exciting to see how it will evolve in the coming years,” he concluded.
Dr Ferrari presented at the 40th Congress of the ESCRS in Milan.
Stefano Ferrari PhD currently serves as Head of Research and Development at the Veneto Eye Bank Foundation in Venice, Italy (http://www.fbov.org). stefano.ferrari@fbov.it
Latest Articles
Towards a Unified IOL Classification
The new IOL functional classification needs a strong and unified effort from surgeons, societies, and industry.
The 5 Ws of Post-Presbyopic IOL Enhancement
Fine-tuning refractive outcomes to meet patient expectations.
AI Shows Promise for Meibography Grading
Study demonstrates accuracy in detecting abnormalities and subtle changes in meibomian glands.
Are There Differences Between Male and Female Eyes?
TOGA Session panel underlined the need for more studies on gender differences.
Simulating Laser Vision Correction Outcomes
Individualised planning models could reduce ectasia risk and improve outcomes.
Need to Know: Aberrations, Aberrometry, and Aberropia
Understanding the nomenclature and techniques.
When Is It Time to Remove a Phakic IOL?
Close monitoring of endothelial cell loss in phakic IOL patients and timely explantation may avoid surgical complications.
Delivering Uncompromising Cataract Care
Expert panel considers tips and tricks for cataracts and compromised corneas.
Organising for Success
Professional and personal goals drive practice ownership and operational choices.