Learning from Experience
Liliana Werner recalls 25 years of ophthalmology findings in AAO Kelman Lecture.

Howard Larkin
Published: Wednesday, February 1, 2023
Howard Larkin reports.
As a PhD student a quarter century ago, Liliana Werner MD, PhD made an important discovery about a Teflon coating applied to polymethyl methacrylate (PMMA) intraocular lenses (IOLs). In vitro, the highly hydrophobic coating showed significant antiadhesive and antiproliferative action against lens epithelial cells (LECs), presumably discouraging posterior capsule opacification (PCO).
“However, when we implanted the coated IOLs in rabbit eyes, it became quite evident other factors may play a role in PCO prevention, such as the IOL design,” Dr Werner said in her Charles D Kelman Lecture “25 Years Evaluating New IOL Technology and Complications” at the American Academy of Ophthalmology 2022 annual meeting in Chicago, US. She is the first woman selected to deliver the prestigious talk.
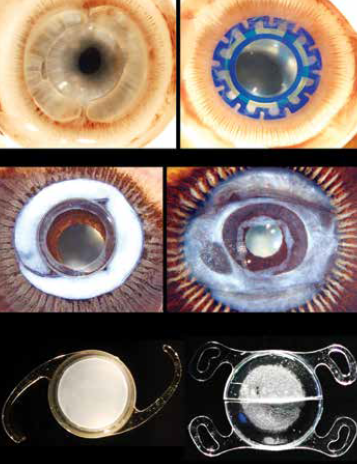
The discovery proved just the start of a series of pioneering studies using in vivo animal models, cadaver eyes, and explanted IOLs (Figure 1) that often yielded surprising findings. Insights generated by the work of Dr Werner and her colleagues guided much of the materials, design, and implantation methods seen in today’s most advanced techniques and devices.
Controlling PCO
After earning her PhD with a thesis based on discouraging PCO with antiadhesive materials, Dr Werner joined David J Apple MD’s ophthalmic pathology lab, where one of the first studies she was involved with tested the opposite hypothesis—promoting the adhesion of the capsule with a monolayer of LECs to bio-adhesive IOL surfaces could prevent further cell proliferation. Similar research later helped bring down PCO even with microincision IOLs notorious for high rates, she said.
With standard IOLs, though, a square edge on the posterior surface proved to play the most prominent role in PCO prevention, Dr Werner said. Cadaver eyes demonstrated that lenses with sharp posterior edges discouraged PCO regardless of material.
Dr Apple’s six factors to prevent PCO summarised this research. Three factors are surgery-related: hydrodissection-enhanced cortical clean-up, in-the-bag IOL fixation, and capsulorhexis smaller than the IOL optic diameter. And the other three are IOL-related: biocompatible materials to reduce LEC proliferation stimulation, contact between the IOL optic and the posterior capsule, and a square IOL optic edge. Using these allows for the capsule to shrink-wrap around the optic of lenses with a more standard design.
However, further research with a bag-filling dual-optic silicone lens showed keeping the bag open and expanded allowed for circulation of aqueous humour within the capsular bag, Dr Werner said. Recently, an open-bag silicone modular accommodating lens showed no PCO in a rabbit model and out to 12 months in human patients.
On the other end of the spectrum, the bag-in-lens—in which the twin capsulorhexes edges fit into a groove around the IOL optic—also completely prevents PCO by sequestering residual LECs in the closed bag around the periphery.
Explanted IOLs
Dr Werner has participated in many studies of explanted IOLs, notably looking for reasons some hydrophilic acrylic lenses tend to calcify. Multiple factors may be at play, some related to manufacturing and packaging using silicone products and others patient-related.
Silicone lens calcification occurs on the posterior optic surface in eyes with asteroid hyalosis. They often reaccumulate, even after partial removal with Nd:YAG laser. The impact on light scatter, light transmission, and modulation transfer function are clinically significant, requiring explantation, Dr Werner said.
Opacification of silicone lenses within a few hours of implant occurred thanks to industrial cleaning and fumigant chemical contamination, which Dr Werner found may have been caused by improper storage. Analysis of some lenses explanted due to toxic anterior segment syndrome (TASS) revealed the presence of ointment used after implantation coating the corneal endothelium and the silicone IOL optic.
Dr Werner examined hydration-related issues in hydrophobic acrylic lenses in which fluid-filled vacuoles known as glistenings form. However, she said glistenings and subsurface nanoglistenings do not affect light scatter and light transmittance enough to require explant in most cases. More recent hydrophobic acrylic lenses with higher water content, ranging up to 4.9%, are much less subject to this phenomenon.
“I could confirm that some of these materials are glistening- free,” she said.
Analysis of explants due to late in-the-bag dislocations showed an association with pseudoexfoliation, uveitis, myopia, pars plana vitrectomy, and other conditions causing progressive zonular weakening rather than any IOL material or design issue. Lenses implanted with a capsule tensioning ring may dislocate sooner, though this may partially be due to the selection of patients with existing zonular problems and additional stress during implantation of the ring itself, Dr Werner noted.
This year Dr Werner and team published on dead bag syndrome, in which the capsular bag becomes diaphanous, floppy, and unable to support the IOL. Analysis of the specimens included in this first study showed scarce or no LECs or proliferative or fibrotic capsule changes, but delamination of the capsule at the zonular attachments.
“Other studies are necessary to fully understand the aetiology and manifestations of this complication,” she commented.
In conclusion, Dr Werner outlined three lessons she learned from 25 years of research on IOL design, materials, and technique. First, keep an open mind because today’s idea may become the next disruptive technology. Second, use a thorough scientific process to ensure clinical practice can safely adopt new ideas. Third, constant vigilance is required to detect and learn from IOL complications, so reporting and analysing them is essential to protect patients—the goal of her life’s work in ophthalmology research.
Liliana Werner MD, PhD is professor of ophthalmology and visual sciences and co-director of the Intermountain Ocular Research Center at the Moran Eye Center of the University of Utah, Salt Lake City, US, and associate editor of the Journal of Cataract and Refractive Surgery. liliana.werner@hsc.utah.edu
Latest Articles
From Lab to Life: Corneal Repair Goes Cellular
Long-awaited cellular therapies for corneal endothelial disease enter the clinic.
Balancing Innovation and Safety
Ensuring access to advanced cell therapies amid regulatory overhaul.
With Eyes on Its Future, ESCRS Celebrates Its Past
Winter Meeting offers opportunities to experiment with new concepts and formats.
Best of ESCRS Winter Meeting 2024
Following the New Generation
EDOF IOLs an option for eyes with mild comorbidities, showing potential in mini-monovision strategies.
Refocus on Multifocals
Trifocal IOLs continue to improve as consensus grows regarding indications and contraindications.
Common Myths in Presbyopia Correction
Patient education key to satisfaction with refractive IOLs.
Reversible Multifocality
Two-lens combination offers low-risk spectacle independence for cataract patients and presbyopes.
Managing a Cataract Surgery Refractive Miss
Weighing the pros and cons of options for intraocular intervention.
Unleashing OCT’s Full Potential
Performance of newest tool for corneal evaluation meets or beats older standard technologies.