Cataract
Is FLACS Worth the Cost?
Femto laser-assisted cataract surgery compared to PCS may not yet justify reimbursements.

Timothy Norris Reports
Twelve years since its introduction, femto laser-assisted cataract surgery (FLACS) is still struggling to par with the cost-effectiveness of the reliable and standardised phacoemulsification cataract surgery (PCS), making it difficult to justify funding by private and public healthcare system reimbursements.
Today, many enthusiastic advocates praise the clean, elegant, and precise FLACS, enabling fast and easy high standard capsulotomies and the potential to improve postoperative refractive outcomes. While recognising the undeniable slow adoption rate, many consider FLACS a great option for their future clinical practice. However, the initial promise of replacing PCS as the primary choice worldwide has never really fulfilled, instead placing it at risk of losing the race against its standardised counterpart.
The femtosecond laser-assisted versus phacoemulsification cataract surgery (FEMCAT) study published in 2020 concluded that considering the higher costs, the femtosecond laser-assisted procedure does not provide an advantage over conventional PCS.1
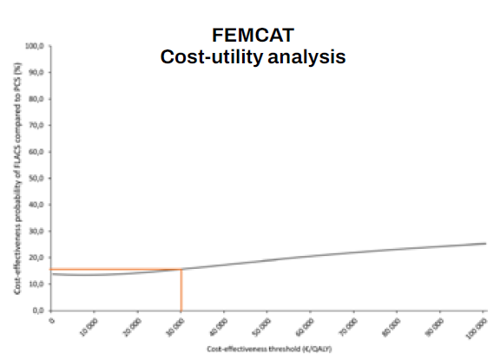
More recently, a preplanned cost-utility secondary analysis of the FEMCAT trial went deeper into the issue of the cost-effectiveness of FLACS on a 12-month time horizon, thoroughly evaluating the micro-costing and utility of both procedures. The authors concluded that in its current state, FLACS is “not cost-effective and should not be reimbursed by healthcare systems,” pointing to investment in research and development as the only worthwhile option for its future.2
Study results showed that the Institute for Clinical and Economic Review (ICER) of FLACS compared to PCS was not within the €45,000 to €89,000 per QALY range frequently cited as cost-effective, confirming the FEMCAT trial findings.
“We showed in the FEMCAT study that the direct cost of cataract surgery was [more than] €500 in the FLACS group, with only a small health benefit for patients compared to the PCS group,” Dr Cedric Schweitzer, first author of the FEMCAT study, said in an interview for EuroTimes.
“We found the cost-effectiveness priority of FLACS compared with PCS phaco did not exceed 15% for a cost-effectiveness threshold commonly recognised in Europe at €30,000 per QALY gained.”
He reaffirmed more research and development will be required to narrow the gap between the two procedures, improving FLACS’s effectiveness and lowering the costs.
“FLACS is a ground-breaking technology, and despite being still in its infancy stage, it is already at par with its much older counterpart in efficiency. Overall, the results of the FEMCAT trial and secondary cost-utility analysis are not negative for the femtosecond laser-assisted cataract surgery, but the quantitative information on the added benefit for patients and the additional direct and indirect cost of each procedure can be invaluable for all the actors involved,” he said.
“We still need further improvements—both in surgical technology and IOL design—if we want to translate the very precise cut of femtolaser into solid clinical benefit.”
In an invited commentary on the secondary analysis, Professor Oliver D Schein stated that, given the findings of his French colleagues, “it remains unlikely that FLACS in its current incarnation would be funded by federal or private insurers in the US.”3
Ironically, if those insurers did cover it, the rate of FLACS procedures would fall dramatically in the country, he pointed out. “From the perspective of the surgeon, an extra $300 per case would probably not justify the extra time and expense of FLACS, especially in the known absence of clinical benefits.”
Finding an agreement between stakeholders about direct and indirect costs may very soon become necessary to avoid such a negative scenario.
“By measuring the cost of each surgical procedure, we provided valuable information [available] to develop a suitable economic model for this technology,” Dr Schweitzer said.
With the results of these studies, “each company and decision maker can play on the price of each part of the surgery to narrow the gap and make FLACS a better choice than PCS,” he concluded.
For citation notes, see page 40.
Cedric Schweitzer MD is a professor of ophthalmology at the University of Bordeaux, France. cedric.schweitzer@u-bordeaux.fr
Latest Articles
Towards a Unified IOL Classification
The new IOL functional classification needs a strong and unified effort from surgeons, societies, and industry.
The 5 Ws of Post-Presbyopic IOL Enhancement
Fine-tuning refractive outcomes to meet patient expectations.
AI Shows Promise for Meibography Grading
Study demonstrates accuracy in detecting abnormalities and subtle changes in meibomian glands.
Are There Differences Between Male and Female Eyes?
TOGA Session panel underlined the need for more studies on gender differences.
Simulating Laser Vision Correction Outcomes
Individualised planning models could reduce ectasia risk and improve outcomes.
Need to Know: Aberrations, Aberrometry, and Aberropia
Understanding the nomenclature and techniques.
When Is It Time to Remove a Phakic IOL?
Close monitoring of endothelial cell loss in phakic IOL patients and timely explantation may avoid surgical complications.
Delivering Uncompromising Cataract Care
Expert panel considers tips and tricks for cataracts and compromised corneas.
Organising for Success
Professional and personal goals drive practice ownership and operational choices.