Cataract, Refractive
Common Concerns with Refractive IOL Procedures
Expanding IOL choices increase treatment options

Sean Henahan
Published: Thursday, June 1, 2023
Sean Henahan reports
Who should be considered for presbyopia-correcting IOLs and who should not? Panellists addressed a series of key issues surrounding this question during a symposium at the ESCRS Winter Meeting in Vilamoura, Portugal.
Current estimates suggest 10% of cataract patients have glaucoma. The first question to the panel addressed the suitability of implanting presbyopic correcting IOLs in patients with glaucoma. A preliminary audience survey showed strong reluctance, with 68% opting not to use these lenses in glaucoma patients.
“We need to consider what we mean by glaucoma—severe glaucoma with visual field defects is different than, say, a little hypertension, and are controlled with drops,” said Professor Thomas Kohnen. “Nowadays, we have many more options to keep the pressure down over the long term.”
Professor Oliver Findl noted the importance of contrast sensitivity in these patients, saying that even if there is a patient with ocular hypertension, full visual fields, and normal optic nerve, or a patient with very early disease with no reduction in the visual field, contrast sensitivity issues can still appear later.
“These patients have a high life expectancy. When we operate on a 65-year-old, they may live another 20 or 25 years,” he commented. “We don’t know how the glaucoma will progress over that time. You generally don’t want a lens that will compromise contrast sensitivity, so it also depends on which type of presbyopia-correcting IOL you are talking about.”
Prof Kohnen concurred, adding, “We now have a variety of presbyopia-correcting IOLs. From monofocal plus and EDOF lenses to diffractive multifocal IOLs. I would aim most of the time for non-diffractive EDOF lenses because you have a lower chance of contrast sensitivity loss.”
Presbyopia IOLs for retinal disease?
The panel next addressed presbyopia IOL use in patients with retinal pathology. A majority of the audience, 86%, opposed the idea. Contraindications for presbyopia lenses in this group include severe retinal pathology or disease, patient age, and visual status.
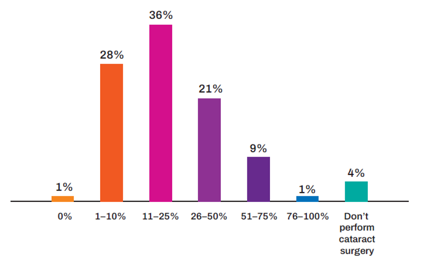
What percentage of your cataract patients present as asymptomatic of any ocular surface disease prior to surgery but develop symptoms postoperatively?
“There is a broad spectrum of retinal pathology. There are restrictions, but I would not say it is an absolute no-go. Trifocal IOLs are a no, but monofocal plus IOLs might be a good option in some cases,” Prof Kohnen said. “An EDOF lens might be considered, depending on which type, though never a diffractive lens.”
Ocular surface disease is not uncommon in cataract patients. The panellists agreed OSD should be managed first before considering presbyopic lens options.
“We need to do the diagnostics. This is more important than ever. You have to look not only at the tear film but at the thickness of the epithelium,” Prof Kohnen explained. “For me, severe OSD is always a contraindication. In milder cases, I support pretreatment and multiple diagnostic assessments. Then I would go with a more forgiving lens.”
Night vision problems
Night vision dysphotopsia continues to be one of the most prominent concerns among potential presbyopia IOL patients.
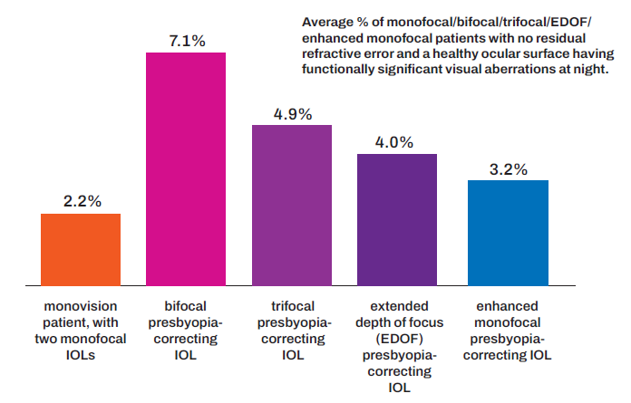
“The average percentage of patients with no residual refractive errors and healthy ocular surface who go on to have postop aberrations ranges from 5–7%. It is higher for bifocal and trifocal lenses,” Prof Findl told the symposium. “From our perspective, it is really important to inform patients beforehand that they may encounter these symptoms, depending on the type of IOL. With a trifocal, for example, you will definitely expect halos, maybe less so with an EDOF lens.”
Prof Kohnen added the challenge now is matching the IOL to the patient.
“You have to manage expectations. If I have a patient who has to drive five times per week from Frankfurt to Munich at night, I would probably not give him a trifocal lens. I would go for a non-diffractive EDOF,” he said. “But you have to remember many patients do not have this problem with trifocal IOLs.”
Neuroadaptation is another piece of the puzzle in these cases. Prof Kohnen and his group have completed a study, now in press, that concludes halos—the most bothersome aspect of dysphotopsia—tend to diminish in some cases between three and six months after surgery.
Should monofocal plus IOLs should be the new standard monofocal IOL?
“It really depends on our healthcare systems. If monofocal plus has better outcomes, then they really should replace standard monofocals. But you need healthcare systems to adopt—and possibly pay more—for them,” Prof Kohnen said.
Prof Findl responded enhanced monofocals are essentially the same price in his country, Austria, and they have become the standard choice for all his patients.
Oliver Findl MD, MBA, FEBO is the Chair of the Department of Ophthalmology, Hanusch Hospital, Vienna, Austria. He is the current president of the ESCRS. oliver@findl.atThomas Kohnen MD, PhD, FEBO is professor and chairman, Department of Ophthalmology, Goethe University, Frankfurt, Germany.kohnen@em.uni-frankfurt.de