Combined Surgery for Cataract and ERM—Yes or No?
ESCRS symposium looks to the future of ophthalmology.

Howard Larkin
Published: Monday, July 4, 2022
Better patient visual outcomes, safety, and convenience favour combined surgery, though refractive considerations may warrant a sequential approach.
Howard Larkin reports from the 2022 ASCRS Annual Meeting
If a patient has both a cataract and an epiretinal membrane (ERM), and one is minimal, should both be addressed in a combined procedure, or should they be handled sequentially? Christina Y Weng MD, MBA and Richard Tipperman MD debated the pros and cons.
Arguing for a combined approach, vitreoretinal surgeon Dr Weng asked, “Why risk a suboptimal outcome? We know that patient expectations are higher than ever. If you only do one, you risk not meeting those expectations.” She gave three reasons to consider combined surgery.
Anterior segment surgeon Dr Tipperman mostly agreed with Dr Weng but suggested refractive considerations may warrant a sequential approach. He offered a simple algorithm for selecting patients for combined surgery.
BETTER TOGETHER
Dr Weng’s first reason for combining surgeries was that doing only one surgery often leads to a suboptical visual outcome due to the other pathology. For example, if only the cataract is treated, patients may still have metamorphopsia, blurriness, or worsened cystoid macular oedema (CME) from the ERM. If only the ERM is treated, virtually 100% will see their cataract worsen after vitrectomy, usually in the first year or two.
Backing her point, Dr Weng cited a study finding post-cataract surgery CME rates were more than six times higher in 812 eyes left with primary ERM than in more than 159,000 reference eyes without ERM.i Patients undergoing combined surgery also achieved their best-corrected visual acuity 15 months sooner when compared to sequential surgery with similar complication rates and greater cost-effectiveness.ii As a bonus, she said combined surgery eliminates floaters that often worsen after cataract surgery and IOL implant.
Second, combined surgery is safe. With today’s small-gauge instruments, the risk of retinal tear or detachment from vitrectomy is less than 2%, and endophthalmitis risk is 0.03–0.11%. There is no evidence combined surgery increases CME, Dr Weng noted.iii
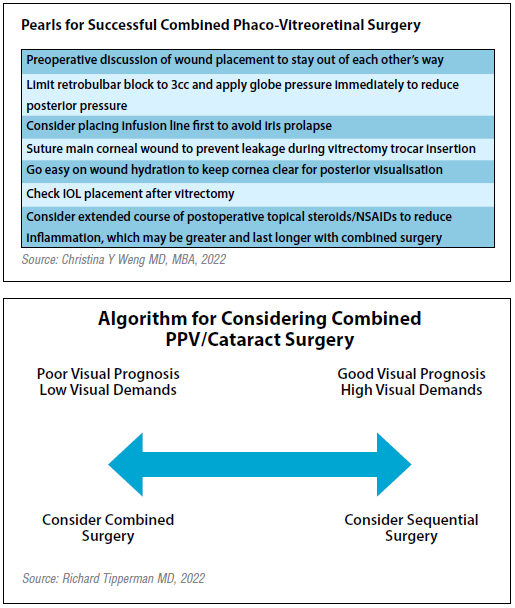
Third, with planning between the two surgeons, the procedures do not have to interfere with each other, Dr Weng said. She recommended a preoperative discussion of wound placement, limiting retrobulbar block volume to reduce posterior pressure, placing an infusion line first to avoid iris prolapse, suturing corneal wounds to prevent leakage during vitrectomy, and going easy on wound hydration to prevent corneal clouding.
“Not only is combined surgery safe and likely to improve visual outcomes, but doing the two surgeries together is no harder – and arguably easier – than doing them separately,” Dr Weng said.
“My patients are happy to have to two-in-one surgery that meets their expectations. . . . Combined surgery is a really great approach for the right patients.”
REFRACTIVE CONSIDERATIONS
While acknowledging Dr Weng’s points, Dr Tipperman noted the decisions required for successful cataract refractive surgery could sometimes tip the scales in favour of a sequential vitreoretinal then cataract approach. He offered five reasons.
First, significant ERM can degrade patients’ fixation ability, which compromises axial length measurement and, therefore, IOL power calculation accuracy. Peeling first may improve fixation and visual outcomes for those with mild ERM.
Second, some patients have a hard time understanding the difference between blur from cataracts and blur from residual metamorphopsia from macular changes, particularly patients with previous macular hole surgery.
“If you peel first and give it a chance to settle down before doing cataract surgery, they have a better understanding of how each pathology affects their vision,” Dr Tipperman said.
Third, while multifocal IOLs are contraindicated for patients with macular pathology, some improve enough after vitrectomy and ERM peeling to become viable candidates. Retinal surgery first allows them to make the decision, he said.
Similarly, patients with ERM and astigmatism may have an easier time judging if paying extra for a toric lens is worth it if the membrane is peeled first. If they end up with poor quality of vision after a peel, it may not be worth it.
Finally, an ERM makes it harder to determine if monovision is an option.
“If they don’t have good vision after peeling, you don’t want to leave them with permanent monovision,” he said.
Patients who form an advanced or mature cataract days or weeks after vitrectomy or intravitreal injection should always have combined surgery, Dr Tipperman said.
“It’s pretty likely the capsule has been violated, and they are going to need a vitrectomy.”
In general, Dr Tipperman’s algorithm suggests those who have a poor visual prognosis and low visual demands should be considered for combined surgery. Those with a good visual prognosis and high visual demands should consider sequential surgery to allow the patient to decide on advanced technology lenses, he concluded.
i JAMA Ophthalmology. 2018 Feb 1; 136(2): 148–54.
ii Graefe’s Archive for Clinical and Experimental Ophthalmology. 2021,
259: 45–52.
iii Retina. 2013; 33(1): 136–42; Retina. 2019; 39(5): 844–52; Graefe’s
Archive for Clinical and Experimental Ophthalmology. 2021 Jul; 259(7):
1731–40. European Journal of Ophthalmology. 2021 Mar; 31(2): 673–8.
Christina Y Weng MD, MBA is associate professor of ophthalmology and director of the vitreoretinal diseases and surgery fellowship program at Baylor College of Medicine, Houston, Texas, USA.
Richard Tipperman MD is an Attending Surgeon and ophthalmologist specialising in refractive surgery, cataract surgery, and management of complications of cataract surgery at Wills Eye Hospital, Philadelphia, Pennsylvania, USA.
Latest Articles
Towards a Unified IOL Classification
The new IOL functional classification needs a strong and unified effort from surgeons, societies, and industry.
The 5 Ws of Post-Presbyopic IOL Enhancement
Fine-tuning refractive outcomes to meet patient expectations.
AI Shows Promise for Meibography Grading
Study demonstrates accuracy in detecting abnormalities and subtle changes in meibomian glands.
Are There Differences Between Male and Female Eyes?
TOGA Session panel underlined the need for more studies on gender differences.
Simulating Laser Vision Correction Outcomes
Individualised planning models could reduce ectasia risk and improve outcomes.
Need to Know: Aberrations, Aberrometry, and Aberropia
Understanding the nomenclature and techniques.
When Is It Time to Remove a Phakic IOL?
Close monitoring of endothelial cell loss in phakic IOL patients and timely explantation may avoid surgical complications.
Delivering Uncompromising Cataract Care
Expert panel considers tips and tricks for cataracts and compromised corneas.
Organising for Success
Professional and personal goals drive practice ownership and operational choices.