Cataract
WSPOS: Complex Cases in Paediatric Cataract

Roberto Caputo MD, from Florence, Italy, discussed the complex problem of paediatric cataract in uveitis during the opening session of the World Society of Paediatric Ophthalmology and Strabismus.
His approach to cataract in these cases is tailored to each patient.
“I ask myself three questions,” Dr Caputo said. “First of all, who is the patient that I am going to treat? When can I do the surgery? And how can I do this surgery?”
Dr Caputo highlighted that cataract in Juvenile Idiopathic Arthritis (JIA) is particularly challenging, with a high risk of complications.
”Can we really wait three months without relapses to do surgery?” he asked. The three month wait is a widespread approach to judging the safe time to wait until cataract surgery in a patient with uveitis, but Dr Caputo questioned whether this is always the best approach, especially in a child with a dense cataract.
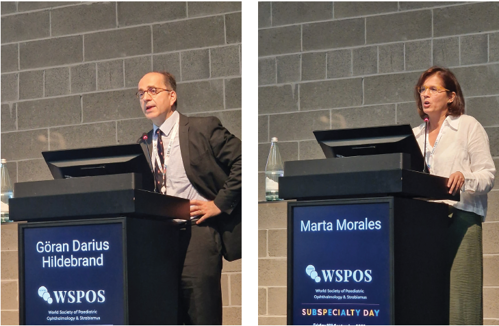
Marta Morales MD, Barcelona, Spain, discussed infant cataract surgery, including some important timing considerations. “It is not recommended to implant an IOL before seven months of age,” she said. “This is in particular due to the risk of visual axis opacification and subsequent requirement for surgery.”
“If we have a dense congenital cataract we should operate as soon as possible, but it is better not to operate before four weeks of age,” Dr Morales continued. “During this age, the anterior segment is still developing.” At this neonatal developmental stage, performing surgery can provoke glaucoma.
Once timing is decided, choosing an appropriate intraocular lens implant is important, taking into account the growth of the eye. There are no paediatric IOL formulae.
“The best formulae are SRKT or Holladay 1,” Dr Morales said. Erick Bothun MD, Rochester, Minnesota, went on to cover cataract surgery in toddlers. “There are challenges in paediatric cataract surgery across the board,” he said. “Most of the literature would suggest that older eyes do better.” The younger the patient, the greater the risk. “There is a higher rate of glaucoma, adverse events, complications.”
“When is it safer to put IOLs in? After six months,” he said. Dr Bothun drew on data from the Toddler Aphakia and Pseudophakia Study (TAPS), drawing comparisons with the Infant Aphakia Treatment Study (IATS). “Largely, glaucoma risk drops off after six months of life.”
Hannah Scanga MD, genetic counsellor at UPMC Pittsburgh, US, talked about the genetics of paediatric cataract. “Your highest diagnostic rate will be found with bilateral cataracts,” Dr Scagna said. Determining a genetic cause starts with history and exam. “Also examine the parents,” she suggested. Important findings can help to narrow down investigation to a causal mutation—for example, findings in mothers who are carriers of Lowe syndrome, such as spoke-like lens changes.
“Genetic causes are being continued to be identified,” Dr Scanga said. “Customisation is helpful.” She suggested a multigene panel as an effective investigative tool.
Göran Darius Hildebrand MD, Oxford, UK, reiterated that paediatric cataract surgery is a vital treatment and that problems arise in postponing surgery. “Delayed surgery leads to permanent brain damage in the form of amblyopia, strabismus and nystagmus.”
Dr Hildebrand was in agreement with Dr Morales that the best formulae available for use in children are SRKT and Holladay 1, as evidenced by a recent meta-analysis, Zhong et al, 2021. But even the best available formulae do not yield results that are comparable to the accuracy of biometry in adults.
“The [rate of] absolute prediction error outside two dioptres reaches 50%.” This error rate is due to numerous factors specific to children, including technical issues obtaining biometry, and childhood emmetropisation.
Dr Hildebrand went on to discuss different approaches to reduce visual axis opacification, highlighting the usefulness of the Bag-In-The-Lens (BIL), invented by Prof. Marie-José Tassignon. For surgeons without access to the BIL, optic capture of a sulcus IOL optic through the anterior and posterior capsule is a potential method to reduce risk of opacification of the visual axis.
Tags: 40th Congress of the ESCRS
Latest Articles
Towards a Unified IOL Classification
The new IOL functional classification needs a strong and unified effort from surgeons, societies, and industry.
The 5 Ws of Post-Presbyopic IOL Enhancement
Fine-tuning refractive outcomes to meet patient expectations.
AI Shows Promise for Meibography Grading
Study demonstrates accuracy in detecting abnormalities and subtle changes in meibomian glands.
Are There Differences Between Male and Female Eyes?
TOGA Session panel underlined the need for more studies on gender differences.
Simulating Laser Vision Correction Outcomes
Individualised planning models could reduce ectasia risk and improve outcomes.
Need to Know: Aberrations, Aberrometry, and Aberropia
Understanding the nomenclature and techniques.
When Is It Time to Remove a Phakic IOL?
Close monitoring of endothelial cell loss in phakic IOL patients and timely explantation may avoid surgical complications.
Delivering Uncompromising Cataract Care
Expert panel considers tips and tricks for cataracts and compromised corneas.
Organising for Success
Professional and personal goals drive practice ownership and operational choices.